-
PDF
- Split View
-
Views
-
Cite
Cite
Naohiro Nose, Tetsuya So, Atsushi Sekimura, Takeaki Miyata, Takashi Yoshimatsu, Subglottic granuloma after aortic replacement: resection via flexible bronchoscopy after an emergency tracheostomy, Journal of Surgical Case Reports, Volume 2014, Issue 9, September 2014, rju088, https://doi.org/10.1093/jscr/rju088
Close - Share Icon Share
Abstract
A subglottic granuloma is one of the late-phase complications that can occur after intubation. It can cause a life-threatening airway obstruction; therefore, a rapid diagnosis and appropriate treatment plan is necessary. A 62-year-old male had undergone an emergency total arch replacement for acute aortic dissection. Postoperative ventilation support had been performed until the 15th postoperative day (POD). He was discharged from the hospital on POD 30. On POD 50, he was brought to our hospital by an ambulance with severe dyspnea. A large subglottic granuloma occupying the trachea was identified by flexible bronchoscopy. After an emergency tracheostomy, resection of the granuloma with argon plasma coagulation via flexible bronchoscopy was performed safely. Physicians should suspect a post-intubation subglottic granuloma when patients who have undergone intubation report feeling throat discomfort. Resection via flexible bronchoscopy after tracheostomy is a safe and feasible procedure that may shorten the duration of therapy and hospital stay.
INTRODUCTION
A laryngeal granuloma is one of the late-phase complications that can occur after intubation [1]. Although it is a rare entity, all surgeons who perform operations under general anesthesia and physicians who treat patients on ventilation may encounter the condition. It can cause a life-threatening airway obstruction; therefore, a rapid diagnosis and appropriate treatment is necessary. There have been some case reports indicating that such a granuloma can be resected by laryngosurgery [2–4]. However, performing laryngosurgery is difficult for non-otolaryngologists. We herein report the successful resection of a subglottic post-intubation granuloma after total arch replacement via a flexible bronchoscopy.
CASE REPORT
A 62-year-old healthy male with severe back pain was diagnosed with an acute aortic dissection (Stanford Type A). Emergency surgery was performed with an 8.0-mm ID endotracheal tube. Neither significant findings of the trachea nor any complications related to the intubation were described in the anesthetic records. Total arch replacement via a median sternotomy in the supine posture was performed with no complications. Postoperative intubation was required for ventilation support until the 15th postoperative day (POD). The patient was discharged from the hospital on POD 30. Beginning on POD 45, he started to experience throat discomfort without dyspnea. Although an expectorant (carbocysteine, 1500 mg/day) was prescribed by his primary doctor, symptomatic improvement was not identified. On POD 50, he developed dyspnea, and the symptoms exacerbated quickly. He was brought to our hospital by ambulance.
Upon arrival, he complained of severe dyspnea with inspiratory stridor in his throat. Computed tomography revealed a mass arising from the posterior wall of the trachea (Fig. 1). Bronchoscopy revealed a white subglottic tumor occupying 80% of the tracheal diameter (Fig. 2). We performed an emergency tracheostomy under topical anesthesia, and the symptoms improved dramatically. For 5 days after the tracheostomy, hydrocortisone was prescribed; however, no tendency toward reduction of the mass could be identified during follow-up bronchoscopy. To shorten the treatment period, we performed a resection of the tumor under bronchoscopy 6 days after the tracheostomy.
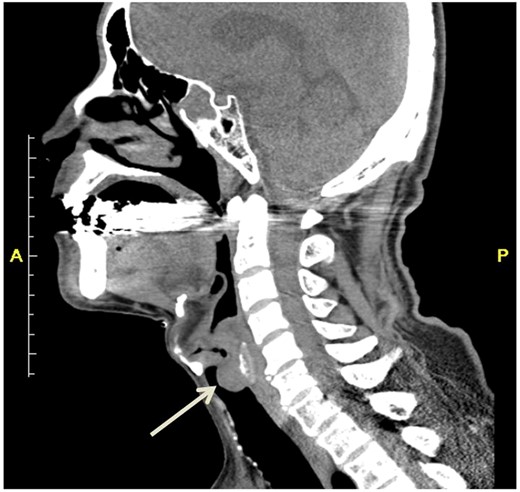
Computed tomography revealed a mass arising from the posterior wall of the trachea (arrow).
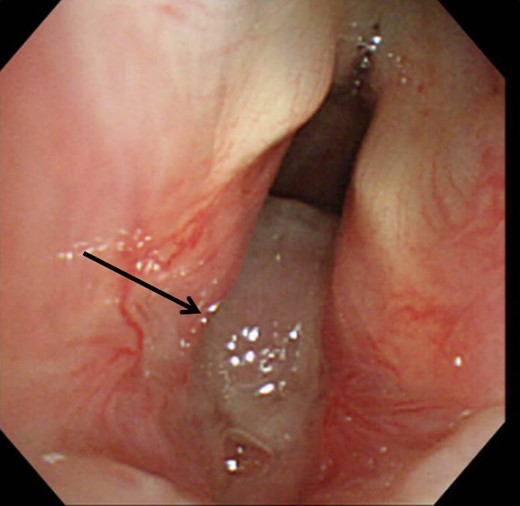
Bronchoscopy revealed a white subglottic tumor occupying 80% of the tracheal diameter (arrow).
The operation was performed with general anesthesia via the tracheostomy tube. The tumor was cauterized with an argon beam coagulator (ERBE VIO-S/APC®) via the bronchoscope, which was inserted from a bite block in his mouth. During the abrasion process, we found that the tumor had a pedicle which could not have been identified by preoperative computed tomography or bronchoscopy. The tumor was resected easily with abrasion of the pedicle. The tracheostomy tube prevented the resected tumor from falling into the distal airway (Fig. 3). Little bleeding was experienced. The total length of the operation was 20 min.
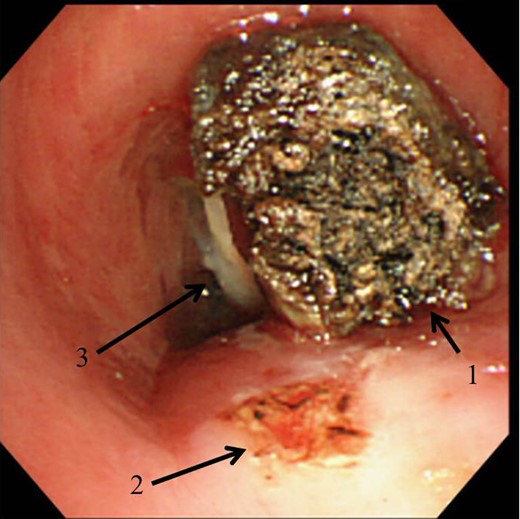
The intraoperative findings: the tumor (arrow 1) was resected by the abrasion of its pedicle, which arose from the tracheal membranous wall (arrow 2). The tracheostomy tube (arrow 3) prevented the tumor from falling into the distal airway.
Three days after the resection of the tumor, the tracheostomy tube was removed. To prevent recurrence, an inhaled steroid was prescribed. He was discharged from the hospital 16 days after the tracheostomy. The inhaled steroid was continued until 3 months after the operation. No recurrence of the tumor was identified by bronchoscopy at 12 months after the resection. The pathological findings of the tumor revealed a granuloma including many lymphocytes, without any malignant component.
DISCUSSION
The rate of post-intubation granuloma formation was reported to range from 0.01 to 3.5% [2]. A higher incidence was reported among females, who are considered to be more susceptible because of the anatomical dimensions of the female larynx, very small stature or obesity accompanied by a short neck were suggested to be risk factors for granuloma formation [2, 3, 5]. Injury and/or friction between the subglottic area and the tube are thought to be the causes of these granulomas [6–8]. Prolonged intubation is also one of the important risk factors [6–8]. However, some case reports have described that this type of granuloma may develop even in patients who were only intubated during the operation [1–4, 6]. All patients who undergo an intubation procedure should be considered candidates for developing this granuloma. The most concerning point of this entity is its acute and life-threatening development 1–12 weeks after the extubation [1, 2, 5, 9]. In this period, most of the patients have been discharged from the hospital. Information that the development of throat discomfort may be a sign of a granuloma should be conveyed to the patients, especially those with many risk factors for this granuloma.
As in our cases, there have been some previous case reports that described the existence of a pedunculated structure [2, 3]. For example, Ozaki et al. [2] reported that a pedunculated granuloma flopped into the subglottic lesion with inhalation and out with exhalation. The acute exacerbation of this granuloma may have be due to its movable structure and the fact that tracheal tumors that are generally asymptomatic until they occlude 50–75% of the lumen diameter [10].
We could only find six emergency cases previously reported in Japanese [2] or English journals [3–5]. In four of the six cases, resection via laryngosurgery was performed with or without tracheostomy. According to these case reports and our experience, the invasiveness of the resection of this granuloma seems to be relatively low. Sugita et al. [5] reported two cases of granulomas that regressed spontaneously by 15 and 17 days after the tracheostomy. Another previous article described the efficacy of conservative therapy, such as voice rest, cessation of smoking, the use of corticosteroids and antibiotics in stable cases [3, 9]. We believe that resection should be considered to reduce the treatment period and to prevent the development of a second granuloma by the tracheostomy tube.
We could not find any previously reported cases in which the granuloma was resected via flexible bronchoscopy. In our case, after the insertion of a tracheostomy tube, the granuloma was separated from the tracheal airway. We believe that when a tracheostomy has already been performed, a procedure via flexible bronchoscopy is safe and feasible even by a non-otolaryngologist. Although we prescribed an inhaled steroid to prevent recurrence, the need for and efficacy of this treatment are unclear. More cases need be accumulated to establish the best treatment for this rare entity.



