-
PDF
- Split View
-
Views
-
Cite
Cite
Nicola Maguire, Bernard Robertson, Philip Henman, Girdlestone procedure for avascular necrosis of the hip in an intravenous drug user, Journal of Surgical Case Reports, Volume 2014, Issue 8, August 2014, rju039, https://doi.org/10.1093/jscr/rju039
Close - Share Icon Share
Abstract
The Girdlestone procedure is an excision arthroplasty of the hip. Rarely used nowadays, it was required in a young patient following discovery of avascular necrosis of the femoral head as a result of septic emboli from infective endocarditis in an intravenous drug user. This procedure was deemed necessary based on poor cardiac function and anaesthetic risk. During this case report we will discuss investigations performed, the procedure and post-procedure course.
INTRODUCTION
The Girdlestone procedure is an excision arthroplasty of the hip, first described in 1945 by Gathone Girdlestone, for the management of tuberculosis and other hip disorders. It is an archaic procedure which has been superseded by total hip replacement and currently has few indications including treatment of infected hip arthroplasty particularly in those elderly patients who are deemed unfit for further revision [1]. The procedure involves resection of a portion of femoral head and neck to allow fusion of the proximal femur with the acetabulum [2]. Functional outcome is poor; however, reduction in pain and removal of sepsis may necessitate this procedure [3, 4].
We will describe an unusual case, where this procedure was used on a young male with infected avascular necrosis of the femoral head.
CASE REPORT
A 23-year-old intravenous drug user, with a complex cardiac history was referred from a district general for further management of a discharging sinus, overlying avascular necrosis of the right femoral head. He presented with a 2-week history of right hip pain and a discharging sinus from the right groin. The patient had a history of methicillin-sensitive Staphylococcus aureus and Group G streptococcus positive infective endocarditis (in 2011) resulting in severe mitral regurgitation for which he was taking long-term flucloxacillin. Mitral valvuloplasty was discussed; however, required cessation of intravenous drug use and consideration of anaesthetic risk. Further complicating his history the patient was on low-molecular-weight heparin for bilateral deep venous thrombosis, had previously suffered hypoxic encephalopathy secondary to drug use and on this admission was confirmed hepatitis-C positive.
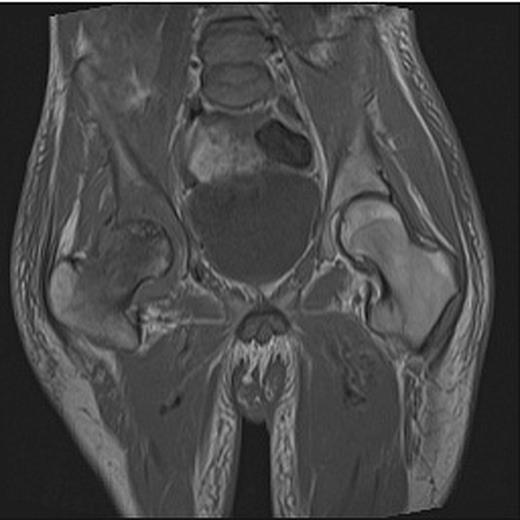
At presentation the patient was afebrile and haemodynamically stable. He was assessed by both the medical and surgical teams at a district general hospital and commenced on intravenous metronidazole and flucloxacillin for a presumed groin abscess. On examination, a pansystolic murmur was heard across precordium with no peripheral stigmata of endocarditis and a discharging sinus in the right groin with a grossly limited range of movement of the right hip. Blood tests revealed a white cell count (WCC) of 7.1 (neutrophils 5.8) and C-reactive protein (CRP) of 146. A pelvic radiograph revealed evidence of degenerative change in the right hip (Fig. 1) and following review by the local orthopaedic team an MRI was carried out confirming avascular necrosis of the right femoral head with an associated collection (Fig. 2).

Pelvic X-ray showing joint space narrowing and collapse of the right hip.
Following a multidisciplinary team discussion at the patient's local hospital consideration was given to his high risk for surgery and anaesthetic due to significant cardiac comorbidity, bilateral lower limb DVTs, poor nutritional status and difficult venous access. The decision was made to transfer to a central teaching hospital by ambulance. The patient was subsequently reviewed by orthopaedics, cardiology, cardiothoracic surgeons, microbiology, infectious diseases and anaesthetics and a plan was made for a Girdlestone procedure. This was to be carried out with experienced cardiothoracic and intensivists available in the event of peri-operative cardiac complications.
A repeat trans-thoracic echo identified new vegetation on the mitral valve and antibiotics were changed to flucloxacillin, rifampacin and metronidazole in keeping with sensitivities from the original episode of endocarditis 2011. Ten days following admission and pre-operative optimization the patient underwent a Girdlestone procedure under general anaesthetic. He returned initially to the high dependency unit as a precaution, before being transferred back to ward-level care.
The patient remained apyrexial during admission and seven sets of blood cultures were negative. Swabs/biopsies taken from his necrotic femoral head in theatre grew Actinomycesodontolyticus and Pantoea agglomerans sensitive to amoxicillin and cotrimoxazole. Following review by infectious disease his antibiotics were changed to amoxicillin, cotrimoxazole and metronidazole in accordance with sensitivities. The patient remained stable post-operatively and was transferred back to his local hospital for ongoing intravenous antibiotic therapy and rehabilitation. His WCC was 4.8 and CRP 65 and decreasing at discharge.
DISCUSSION
This case is interesting for two reasons. First, this procedure is rarely carried out in a young patients due to the unacceptable functional outcome in comparison with newer arthroplastic techniques. A recent review article by Cordero highlighted a few absolute and relative indications for performing this procedure. Intravenous drug use was described as a relative indication, and unacceptable anaesthetic and surgical risk was described as an absolute indication. This young man with a complicated medical history was transferred to a tertiary referral centre to undergo rigorous pre-operative planning and optimization pre-operatively. Active endocarditis was identified in his pre-operative investigations. This case was discussed by several orthopaedic consultants including hip specialists and a consensus was reached to perform the Girdlestone procedure.
Secondly, we propose that avascular necrosis may have occurred as a complication of septic emboli from his active mitral valve endocarditis. A computed tomography chest carried out pre-operatively revealed bilateral upper lobe consolidations in keeping with pulmonary actinomyces infection which may have also originated from the mitral valve vegetation. We are of the opinion that infective seeding may have occluded the vasculature to his femoral head and caused the resultant avascular necrosis and infection. Blood cultures during this admission showed no growth; however, the patient had been on prophylactic flucloxacillin since 2011 and intravenous antibiotics were commenced prior to any blood cultures being taken on this admission. It was also noted that as per hospital policy blood cultures were taken in aerobic bottles and this may be a reason as to why actinomyces may not have been cultured.
This patient was complex and interesting and required input from several specialties within a teaching hospital. He did remarkably well post-operatively without any serious complications.



