-
PDF
- Split View
-
Views
-
Cite
Cite
Astrid A.M. Huiberts, Sandra C. Donkervoort, Willem L. Blok, Hans L.G. Blaauwgeers, Enterocolic lymphocytic phlebitis: an oncologic surgical resection without a preoperative pathologic diagnosis, Journal of Surgical Case Reports, Volume 2014, Issue 5, May 2014, rju037, https://doi.org/10.1093/jscr/rju037
Close - Share Icon Share
Abstract
A patient with complaints of an abdominal (mesenteric) mass is presented. Differential diagnosis included neoplastic processes, such as malignant lymphoma, desmoid tumour, a carcinoid or a gastro-intestinal stromal cell tumour. An oncological resection was performed. Despite the malignant appearance of the tumour no malignancy was found with histopathological examination. Vasculitic lesions were seen in venous structures, resembling veno-occlusive disease with signs of recanalization and with the presence of inflammatory cells, mainly lymphocytes. A diagnosis of enterocolic lymphocytic phlebitis was made. This benign condition can mimic malignancy, necessitating a wide excision, also because obtaining a pre-operative histopathological diagnosis is hardly possible.
INTRODUCTION
Enterocolic lymphocytic phlebitis (ELP) is a disease entity characterized by lymphocytic inflammation of the bowel wall and mesenteric veins and venules, without arterial involvement and without evidence of systemic vasculitis. The term has been first described by Saraga et al. in 1989 [1], although earlier reports seem to have described the same entity [2].
CASE REPORT
A 42-year-old—previously healthy—female was referred to the surgical outpatient clinic because of an abdominal (mesenteric) mass. She had been evaluated by the gastroenterologist because of abdominal pain that had been present for some weeks, forcing her to take analgetics. There was no history of previous abdominal complaints and the pain could not be induced by movement or eating. Stools were normal, without blood or mucus. The patient had lost some weight with a diet, but otherwise intake was normal. A couple of days before presentation she complained of nausea, without vomiting. She also suffered from hot flashes and night sweats.
An ultrasound of the abdomen revealed a tumourous mass in the left lower quadrant of the abdomen. On computed tomography (CT) scan and MRI this appeared to be a tumour in the radix mesenterii (Fig. 1a and b). The differential diagnosis included neoplastic processes, such as malignant lymphoma, desmoid tumour, a carcinoid or a gastro-intestinal stromal cell tumour.
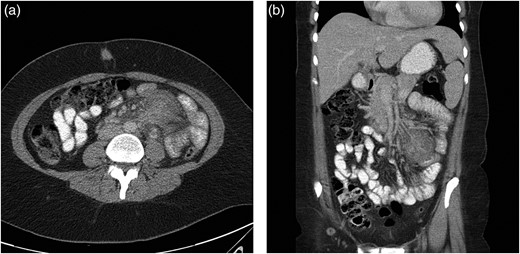
(a) Transverse CT image with the ill-defined tumour in the left side of the patient. (b) Coronal CT image showing the same ill-defined tumour.
Explorative laparoscopy was converted to an open procedure because of the macroscopic malignant aspect of the tumour. The mesentery of the sigmoid was involved and had to be resected en bloc with the sigmoid and part of the jejunum. Radical, oncological resection with stapled anastomoses was performed. The patient recovered slowly but uneventfully.
A pathology report surprisingly showed no malignancy; the resection specimen consisted of a 40 cm long part of small bowel and the sigmoid connected to one another by thickened, tumorous-appearing mesentery. On cross section an ill-defined mass was seen, extending in the bowel walls, with near ulceration of the overlying small bowel mucosa (Fig. 2).

Histopathological examination showed no malignancy. In the tumorous mass, organizing granulation tissue was present. Vasculitic lesions were seen in venous structures, resembling veno-occlusive disease with signs of recanalization and with the presence of inflammatory cells, mainly lymphocytes (Fig. 3). A diagnosis of ELP was made.
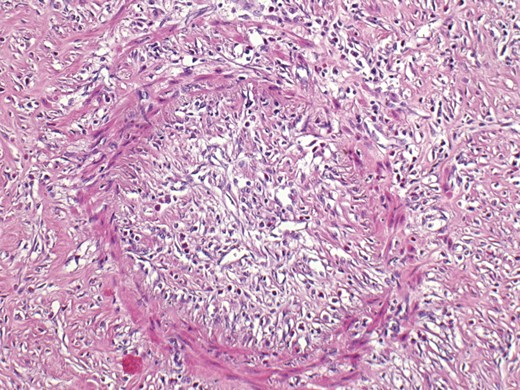
Microscopic appearance with the presence of inflammatory cells, mainly lymphocytes.
DISCUSSION
A diagnosis of ELP is predominantly made after histological resection, since the diagnosis relies on the presence of submucosal venules in biopsy specimens. Most biopsies present mucosa but not submucosa and therefor no classifying diagnosis can be made on biopsy alone. No pathognomonic features are present on ultrasound or CT imaging. Presentation of ELP with a tumour-like mass is rare but has been described [3]. Also in this case the tumorous mass was highly suggestive for malignancy.
ELP has a wide range of clinical and histological presentation [6, 8, 9]. Clinical presentation can range from long-standing abdominal complaints with a sudden (sub)acute worsening of complaints [3] to presentation with an acute abdomen [4]. Histological features can range from a granulomatous phlebitis, a necrotizing phlebitis to myointimal and endothelial hyperplasia often accompanied by venous thrombi [5].
Aetiology and pathophysiology are unknown but a possible relation with a delayed type hypersensitivity reaction has been postulated [3, 4]. In concordance with this some medication have been related to ELP, e.g. flutamide and rutoside [5, 7]. In our patient none of these possible associations was present. There were also no signs of a systemic vasculitis.
This benign condition can mimic malignancy, necessitating a wide excision, also because obtaining a pre-operative histopathological diagnosis is hardly possible.



