-
PDF
- Split View
-
Views
-
Cite
Cite
Chunseok Yang, Daedong Kim, Small bowel obstruction caused by sigmoid mesocolic hernia, Journal of Surgical Case Reports, Volume 2014, Issue 5, May 2014, rju036, https://doi.org/10.1093/jscr/rju036
Close - Share Icon Share
Abstract
Internal hernia is an unusual cause of small bowel obstruction and classified several types according to locations. Sigmoid mesocolic hernia is an uncommon condition and among others intramesosigmoid hernia was rarely reported in the literature. We report the case of a 49-year-old female with a rare type of congenital internal hernia, through the mesosigmoid, causing small bowel obstruction. She suffered from obstructive symptoms but with no previous history of laparotomy. The diagnosis of internal hernia was suggested by computed tomography, but the type of internal hernia was confirmed by laparoscopic exploration. She underwent laparoscopic detachment of peritoneal attachment comprising hernia sac without defect repair. The postoperative course was uneventful and the patient is free from symptoms and recurrence. This report presents a case of intrasigmoid hernia managed successfully by the laparoscopic approach and shows another surgical technique according to hernia types.
INTRODUCTION
Internal hernia is the protrusion of the intra-abdominal viscera through peritoneal or mesenteric orifices within the peritoneal cavity. Internal hernias is an infrequent cause of small bowel obstruction with a reported incidence of up to 5.8% of intestinal obstruction, and paraduodenal hernias representing 50% of the 500 cases published up to the year 2000 [1, 2]. There are several types of internal hernia as traditionally described, according to their location [3].
Sigmoid mesocolic hernia is a rare type of congenital hernia and intramesosigmoid hernia is the rarest amongst the sigmoid mesocolic hernia [4–6]. There are only three previous reports of laparoscopic surgery of sigmoid mesocolic hernia in the surgical literature. We present the case of rare type of congenital internal hernia and managed it successfully by the laparoscopy.
CASE REPORT
A 49-year-old female was transferred to our emergency department with abdominal pain of several hours’ duration. Pain showed colicky and aggravated pattern in the periumbilical area. She had continuous vomiting and no flatus after onset. There was no history of similar previous episodes or any prior abdominal surgery. The abdomen was slightly distended with periumbilical tenderness but soft without peritoneal signs. No inguinal hernias were noted.
Laboratory data were unremarkable. Abdominal X-rays showed slight distension of small bowels with air-fluid levels (Fig. 1). CT scan revealed that dilated small bowel loops probably ileal level in left lower quadrant (Fig. 2). A nasogastric tube was inserted and she was given a conservative treatment over the next 2 days, but we proposed a laparoscopic exploration because of no clinical improvement.

Upright abdominal radiograph showing multiple air-fluid levels, suggestive of possible distal bowel obstruction.
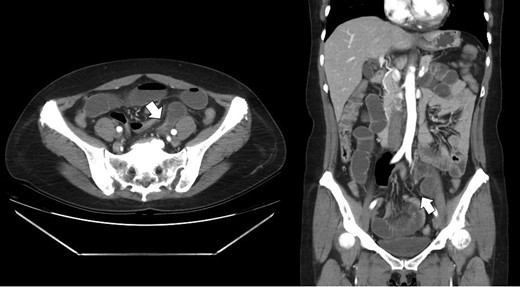
Contrast enhanced CT showing the transitional zone (white arrow) between dilated to collapsed loops in the left lower abdomen.
A laparoscopic approach was performed with the patient under general anaesthesia. A 10-mm port for camera was placed umbilicus by an open method. Two other 5-mm ports were placed for instruments in the right upper and lower abdomen. As tracing retrograde from the ileocecal junction, a loop of mid-ileum was incarcerated to ∼2-cm sized defect lateral to the sigmoid colon. First, trying the reduction of small bowel loop by atraumatic grasper gently, detachment of sigmoid lateral attachment was performed. Incarcerated bowel was released as soon as we detached a just little (Fig. 3). Approximately 15 cm of small bowel had been incarcerated in the defect and initially appeared congested but its colour and peristalsis improved rapidly. The hernia defect did not involve the medial aspect of the peritoneum on the sigmoid mesocolon and was confirmed no full-thickness defect. The defect was disappeared and changed to broad space easily from dissection of peritoneal attachment. There was no need to close the defect by intracoporeal suture laboriously. The operation was finished after confirmation of preventing recurrence. The postoperative course was uneventful and the patient was discharged 5 days postoperatively. The patient is free from recurrence.
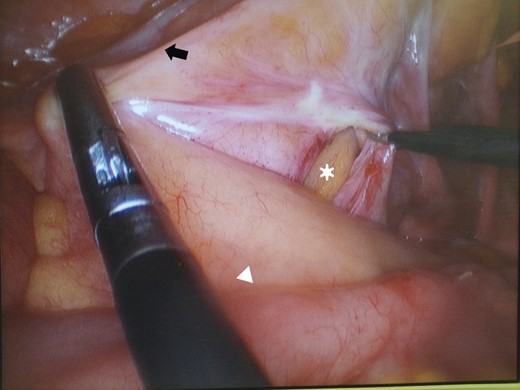
After reducing the incarcerated ileum (white arrowhead), the defect (asterisk) in the lateral leaf of the sigmoid mesocolon (black arrow) is seen.
DISCUSSION
Internal hernia is caused by a defect within the boundaries of the peritoneal cavity. These defects may be congenital, traumatic, postoperative, post-inflammatory or idiopathic. The autopsy incidence of internal hernias is 0.2–2%, most of them is asymptomatic and acquired [1]. The herniated bowel may return to its normal location or be incarcerated, depending on the size of the defect and the length of the herniated bowel [7]. Sigmoid mesocolic hernia although uncommon, it is not extremely rare accounting for 5% of all internal hernias [8].
Benson and Killen [9] classified sigmoid mesocolic hernias into the following three types. (i) intersigmoid hernia: herniation into an intersigmoid fossa, situated at the attachment of the lateral aspect of the sigmoid mesocolon. This fossa is formed during fusion of the left peritoneal surface of the sigmoid mesentery with the parietal peritoneum of the posterior abdominal wall, the line of Toldt. (ii) Transmesosigmoid hernia: incarceration of intestinal loops through a full-thickness defect in the sigmoid mesocolon. (iii) Intramesosigmoid hernia: a congenital, oval defect unrelated to the intersigmoid fossa is present in juxtaposition to the colon and involves only one leaf (lateral more common) of the sigmoid mesocolon and herniation occurs. A normal fusion fascia is present, and the right leaf is intact in this setting. This was the case in our patient and among others, rarest. No clear radiographic sign allows one to distinguish among the three types of intersigmoid hernias, and no precise radiologic differentiation is required because surgical exploration is mandatory [3].
The clinical manifestations of internal hernia range from mild digestive symptoms to acute abdomen, depending on the severity of the obstruction and the presence of incarceration. CT scan is considered to suggest the diagnosis in a patient suspected of having intestinal obstruction. CT findings showed the presence of encapsulated fluid-filled and markedly distended bowel loops protruding toward left lower abdomen accompanied by fat and mesenteric vessels [3]. However, these findings are not pathognomonic and only suggest the diagnosis. In patients presenting with small intestinal obstruction, the absence of an obvious external hernia, history of tuberculosis or of previous surgery should alert the clinician for the possibility of an internal herniation as the cause [5].
Patients with small intestinal obstruction not responding to conservative therapy require surgery. If an internal herniation is suspected, the surgery should be prompt, as strangulation and necrosis of the hernial contents is likely to ensue if the surgery is delayed. Traditionally, such a treatment is undertaken by open surgery in which the contents are reduced from the hernial defect, and resected if necrotic and the defect is closed [5]. However, if no evidence of strangulation or necrosis, a laparoscopic approach is a useful method. In addition, we propose that there is always no necessity to close the hernia defect. If transmesocolic hernia was found, after reduction the hernia defect must be closed preventing recurrence. But as intramesocolic or intermesocolic hernia, detachment of peritoneal attachment for sigmoid mobilization is feasible and usually enough because there is no complete defect, and narrow hernia sac was changed to broad space which was free from incarceration.
In conclusion, this case report shows the diagnostic as well as therapeutic roles of laparoscopy in patient with acute intestinal obstruction and this approach is feasible and valuable even in a rare pathology such as a sigmoid mesocolic hernia. We suggest not to repair any types of sigmoid mesocolic hernia but to manage more easily according to hernia types.



