-
PDF
- Split View
-
Views
-
Cite
Cite
Marco Cianforlini, Mario Marinelli, Isabella Ponzio, Luigi de Palma, Chopart arthrodesis with graft bone from the iliac crest after a traumatic subamputation of the forefoot: surgical technique, Journal of Surgical Case Reports, Volume 2014, Issue 2, February 2014, rju007, https://doi.org/10.1093/jscr/rju007
Close - Share Icon Share
Abstract
We present a 49-year-old man with a traumatic subamputation of the forefoot, associated with lacerated wound in correspondence of the dorsal surface of the right foot, with injuries of tendinous, ligamentous and vascular structures and with the loss of talus head. The patient underwent salvage arthrodesis of the talonavicular and calcanealcuboid joints with graft bone harvested from the iliac crest. The patient was re-evaluated during a clinical and radiographic follow-up. The arthrodesis was consolidated in ∼3 months. There were no infectious problems and the patient has resumed normal work activities. At a sixth month follow-up, the patient had returned to work and remained pain free while walking. Early anatomic reduction, stable fixation and ligament reconstruction are essential for a good outcome. Primary arthrodesis is a viable option for severe midfoot fracture dislocations, because it facilitates rehabilitation and functional recovery and obviates the need for a secondary arthrodesis should arthritis arise.
INTRODUCTION
Midfoot fractures and dislocations are uncommon because of the intrinsic stability of the tarsal structure. The arthrodesis of the talonavicular joint and calcaneal-cuboid joint is technically complex in the presence of bone defect and there is a high incidence of nonunion. Furthermore, in the presence of large skin exposures, the possibility of infection and the consequent negative effect on bone fusion associate the surgical procedure with a high risk of failure [1, 2].
We report a patient, aged 49, with a traumatic forefoot subamputation.
CASE REPORT
In August 2012, a 49-year-old-man presented to our hospital with a traumatic forefoot subamputation after a work accident. The trauma caused a lacerated wound in correspondence of the dorsal surface of the right foot. Radiographs and computed tomography (CT) examination confirmed the diagnosis of the loss of talus head during the trauma (Fig. 1).

AP (a) and lateral (b) radiographs and CT images (c, d) confirm the diagnosis of the loss of talus head during the trauma.
The patient underwent a first-time surgical repair. Abundant washing of the lacerated wound with saline solution and chlorhexidine was done. Injuries of dorsalis pedis artery, tibialis anterior tendon, estensor digitorum longus tendons, peroneus tertium tendon were revealed, with the loss of talus head and with a complex lesion of the talonavicular ligament. Tendinous structures damaged were surgically sutured and subsequently an antibiotic-loaded cement spacer was positioned into the bone gap to re-establish the joint congruence. The foot was put in a cast and kept non-weight bearing for 8 weeks (Fig. 2).

An image of the foot before the first-time surgical repair reveals the injuries of dorsalis pedis artery, tibialis anterior tendon, estensor digitorum longus tendons, peroneus tertium tendon, with the loss of talus head and with a complex lesion of the talonavicular ligament. (a) Tendinous structures damaged were surgically sutured and subsequently an antibiotic-loaded cement spacer was positioned into the bone gap to reestablish the joint congruence (b). AP (c) and lateral (d) radiographs of the foot in the cast after the surgical time.
Two months after the primary surgery, the patient underwent salvage arthrodesis of Chopart joint via double dorsal incision. The patient was placed in a supine position with a support under the ipsilateral hip to allow easy access to the medial and lateral aspects of the foot. A thigh tourniquet was applied.
The skin incision was made along the lateral aspect of the foot, starting at the base of the fourth metatarsal, and extended proximally toward the tip of the fibula, stopping ∼1 cm short of the tip.
The incision was deepened to the extensor digitorum brevis muscle. The capsule of the extensor digitorum brevis was opened, its origin was released and the muscle was reflected distally ∼1 cm distal to the calcaneocuboid joint.
The calcaneocuboid joint was identified and the soft tissue stripped plantarward and dorsally using a periosteal elevator. The articular cartilage was removed from the calcaneocuboid joint using a small, sharp osteotome. Placing a deep retractor into the wound along the dorsal aspect, the lateral aspect of the talonavicular joint opposite the calcaneocuboid joint was identified and articular cartilage was removed.
The medial approach was through a longitudinal incision, starting at the tip of the medial malleolus and carried distally 1 cm past the naviculocuneiform joint. The incision was deepened through the capsular tissues. The capsule and spring ligament were stripped from the navicular (Fig. 3).
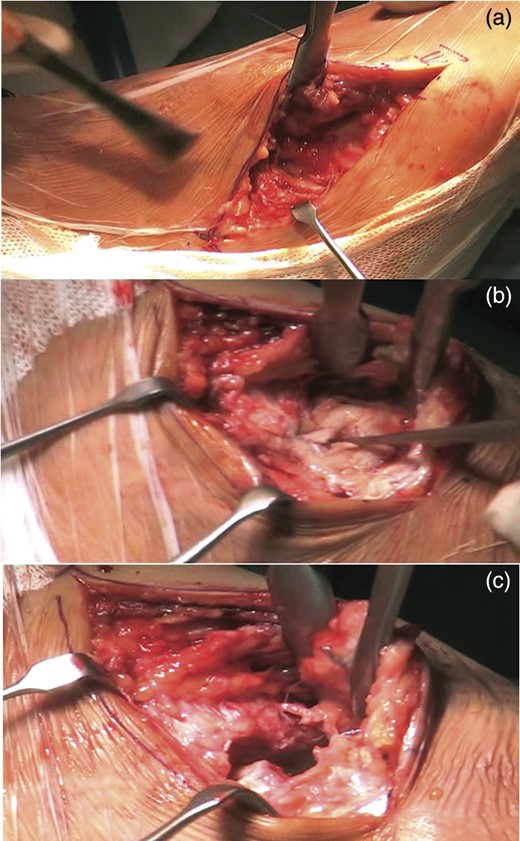
Lateral approach at the base of the fourth metatarsal, and extended proximally toward the tip of the fibula, ∼1 cm short of the tip to identify the calcaneocuboid joint (a). Medial approach through a longitudinal incision, starting at the tip of the medial malleolus and carried distally 1 cm past the naviculocuneiform joint. It is evident of the antibiotic-loaded cement spacer. (b). An elevator was passed over the dorsal aspect of the talonavicular joint. The antibiotic-loaded cement spacer was removed (c).
An elevator was passed over the dorsal aspect of the talonavicular joint, completely freeing the joint. It was removed the antibiotic-loaded cement spacer.
Using a towel clip embedded into the proximal portion of the navicular, the talonavicular joint was distracted by pulling the foot in an adducted position and longitudinally. The articular cartilage was removed from the talonavicular joint with an osteotome.
An autologous graft, harvested from the omolateral iliac crest, was placed into the talonavicular joint [3].
It was evaluated that there was no gap at the calcaneocuboid joint when the foot was brought into a plantigrade position.
Before placing the internal fixation, the bone ends were heavily scaled using a 4 mm osteotome.
The talonavicular joint was fused in situ using two 4.0-mm cannulated screws across the talonavicular joint.
The foot was then manipulated into proper alignment; the guide pin for the 4.0-mm cannulated screw was placed across the talonavicular joint starting at the distal end of the navicular at the naviculocuneiform joint. The placement was checked with fluoroscopy. The navicular was overdrilled with a 4.0-mm drill bit, after which 4.0-mm long threaded screws were inserted.
The fixation of the calcaneocuboid joint was carried out using two 4.0-mm cannulated screws. The screws were brought from proximal to distal, starting in the anterior process area and brought obliquely across into the cuboid (Fig. 4).

The placement of an autologous graft into the talonavicular joint harvested from the omolateral iliac crest (a). The fixation of the calcaneocuboid joint was carried out using two 4.0-mm cannulated screws (b) and the talonavicular joint was fused in situ using two 4.0-mm cannulated screws across the talonavicular joint (c).
The deep layers were closed, followed by the subcutaneous tissues and skin. A compression dressing was applied.
The foot was put in a cast and kept non-weight bearing for 10 weeks, with range-of-movement exercises of the knee and hip allowed. The patient was reevaluated during a clinical and radiographic follow-up at 1, 3, 6 months after surgery. The arthrodesis was consolidated in ∼3 months. There were no infectious problems and the patient has resumed normal work activities [4].
At the sixth month follow-up, the patient had returned to work and remained pain free while walking, with good fusion of both joints (Fig. 5).

AP (a) and lateral (b) radiographs of the foot in the cast after the surgical time. AP (c) and lateral (d) radiographs of the foot at the sixth month follow-up.
DISCUSSION
Dislocations of the midfoot are uncommon because of the constrained configuration of multiple articular surfaces augmented by capsular attachments, strong ligaments and tendons [5, 6].
Foot trauma of this severity can result in articular incongruities, complex derangement of the arc geometry, ligamentous instability, and, eventually, long-term disability secondary to joint subluxation and posttraumatic arthritis [7]. In our patient, the surgical management was based on the principles for treatment of Chopart joint fracture dislocations: realignment of both medial and lateral columns of the foot, restoration of joint congruity, alignment of axes, temporary fixation and ligament reconstruction to ensure proper ligament healing [7, 8].
Early anatomic reduction, stable fixation and ligament reconstruction could have achieved a better outcome [9]. Screws in joint arthrodesis are biomechanically effective for double arthrodesis.
Primary arthrodesis is a viable option for severe midfoot fracture dislocations, because it facilitates rehabilitation and functional recovery and obviates the need for a secondary arthrodesis should arthritis arise. Furthermore, in the presence of large skin exposures, the possibility of infection and the consequent negative effect on bone fusion make the surgical procedure at high risk of failure.
Conflict of interest statement
The authors declare they have no conflict of interests. The manuscript is original, it is not under consideration for publication elsewhere, and has not been previously published. The manuscript has been read and approved by all the authors. The requirements for authorship have been met. Each author believes that the manuscript represents honest work.



