-
PDF
- Split View
-
Views
-
Cite
Cite
Chin Li Tee, Tobias Evans, Sujith Ratnayake, Boris Strekozov, Small bowel obstruction secondary to bilateral obturator hernia: a rare occurrence, Journal of Surgical Case Reports, Volume 2014, Issue 2, February 2014, rju009, https://doi.org/10.1093/jscr/rju009
Close - Share Icon Share
Abstract
Obturator hernia (OH) is a rare type of pelvic hernia. It can cause significant morbidity and mortality, especially in the elderly age group. Delayed treatment is associated with high rates of strangulation (25–100%). We present an 88-year-old woman who presented with symptoms of bowel obstruction and right hip pain. Computed tomography (CT) abdomen revealed bilateral OHs and bowel obstruction secondary to the right OH. She was managed conservatively due to her age and co-morbidities and her bowel obstruction subsequently resolved. She was discharged, only to re-present 1 month later with similar complaints. A repeat CT scan revealed bilateral OHs and bowel obstruction due to the left OH. She underwent midline laparatomy and both OHs were reduced. The right OH was fixed with polypropylene mesh plug and the left OH was fixed with primary closure. The patient recovered and no recurrence was noted during follow-up.
INTRODUCTION
Obturator hernias (OHs) are rare; they represent only 0.05–1.4% of all abdominal wall hernias [1]. The typical patient with an OH is usually a thin, elderly woman. Women are affected nine times more frequently than men, because of broader pelvis with a larger triangular obturator canal opening with a greater transverse diameter, and a history of pregnancy [2]. Additional contributing factors are multiparity, chronic illness, malnutrition and conditions associated with increased intra-abdominal pressure [3].
CASE REPORT
A 88-year-old woman presented to the ED with abdominal pain, vomiting, right hip pain and diarrhoea. Medical co-morbidities include ischaemic heart disease, hypertension and bilateral osteoarthritis of the hip. Her surgical history includes three Caesarean sections, open cholecystectomy, umbilical hernia repair and left mastectomy for breast cancer. A computed tomography (CT) abdomen revealed small bowel obstruction due to the right OH (Fig. 1) and evidence of a small left OH. A trial of conservative management was made for patient due to her age, multiple co-morbidities and patient's wishes. Bowel obstruction resolved with conservative management. The patient re-presented 1 month later with small bowel obstruction and pain radiating down medial left leg. There were no clinical signs of intestinal ischaemia. Abdominal x-ray was consistent with small bowel obstruction (Fig. 2) and CT abdomen revealed transition point at left OH (Fig. 3). A decision was made to proceed with midline laparotomy and bilateral OH repair. Intra-operatively, there was a large right OH containing a small bowel, which was reduced, and a bard polypropylene mesh plug inserted into the defect and fixed with prolene interrupted sutures. The left OH was smaller and was repaired primarily with prolene. The patient made an unremarkable recovery, and she was discharged 3 days after the operation. No recurrence was noted within a year of follow-up.
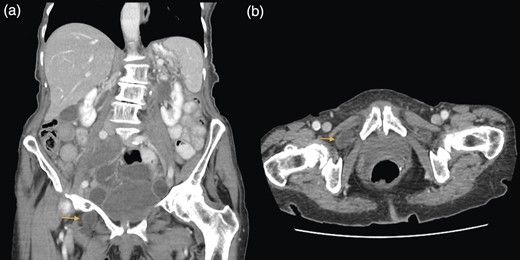
(a and b) Small bowel obstruction secondary to a right OH. (a) Coronal and (b) axial.

Abdominal x-ray showing dilated small bowel loops and severe osteoarthritis changes in both hips.
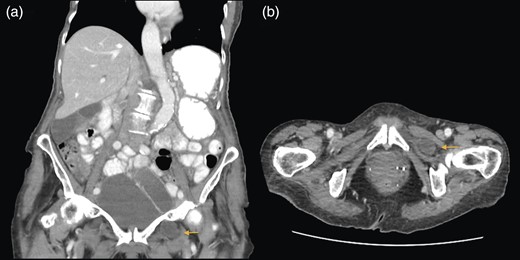
(a and b) Small bowel obstruction secondary to a left OH. (a) Coronal and (b) axial.
DISCUSSION
OH was first described by Arnaud de Ronsil in 1724. It occurs when viscera herniates through the obturator canal, through which the obturator vessels and nerve pass to reach the hip. Three stages of OH formative have been described: (1) pre-peritoneal connective tissue and fat enter the obturator canal; (2) a dimple is formed in the peritoneum over the internal orifice of the obturator canal and progresses to the invagination of a peritoneal sac and (3) viscera, typically ileum, enters the sac [4]. In an emaciated patient, the loss of protective pre-peritoneal fat over the obturator canal increases the risk of herniation [5].
According to a case series of 30 patients by Mayo Clinic, the most common presenting signs and symptoms were bowel obstruction (63%), abdominal/groin pain (57%) and a palpable lump in medial aspect of thigh (10%) [6]. The pathognomonic Howship–Romberg sign, which is pain along the distribution of the obturator nerve, is present in 37% of patients. High morbidity in OH is directly related to the advanced age of the patients, diagnostic delay, gangrene and bowel perforation, deterioration and disability of the patients, and associated chronic diseases [7, 8]. As such, conservative management has little or no place in the management of OH, as is proved in our case where conservative management did eventually fail.
The early diagnosis is challenging when the symptoms and signs are non-specific. Among the various radiologic diagnostic modalities, CT scan has superior sensitivity and accuracy [6], as it allows definitive diagnosis of OH before laparotomy, and it can also show incarcerated bowel in the obturator foramen, with contrast scans having the ability to demonstrate any ischaemia or infarction. In a setting where CT is not available, plain abdominal radiographs can show signs of bowel obstruction, and ultrasound examination may reveal a hypoechoiec mass reflecting a dilated oedematous bowel segment [9].
OH repair is usually accomplished by a midline laparotomy and primary repair. However, with the advent of laparoscopy, additional choices of mesh, and the possibility of a pre-operative diagnosis, other options for repair now exist. Laparoscopic repair is only suitable for elective repairs, mostly when OH presents as an incidental intraoperative diagnosis during a laparoscopic hernia repair or other pelvic operation [6]. A midline laparatomy was applied in this case because it has the advantages of better exposure and facilitation of bowel resection when necessary. We used a prosthetic plug to reinforce the obturator foramen in one side and a simple primary closure for the other side, and the outcome was satisfying. After reduction of the contents, it is necessary to check the viability of the bowel and perform segmental resection of ischaemic or gangrenous areas [9].
In conclusion, OHs are rare and usually present emergently. They should always be suspected when a thin elderly woman presents with symptoms of bowel obstruction or non-specific pain over the thigh and hip. Early diagnosis and prompt surgical treatment are essential to reduce mortality and morbidity.
ACKNOWLEDGEMENT
We would like to thank Caboolture Hospital for its support toward our effort.



