-
PDF
- Split View
-
Views
-
Cite
Cite
Amy Hoi-Ying Pun, Peter G. Devitt, Primary malignant melanoma of the oesophagus: two case reports, Journal of Surgical Case Reports, Volume 2014, Issue 2, February 2014, rju005, https://doi.org/10.1093/jscr/rju005
Close - Share Icon Share
Abstract
Primary malignant melanoma of the oesophagus is a rare and aggressive malignancy. This tumour entity accounts for 0.1–0.2% of all oesophageal malignancies and risk factors are yet to be established, although melanosis of the oesophagus may reflect its precursor form. Dysphagia is the commonest symptom. On gastroscopy, it appears as an elevated pigmented mass with satellite lesions in some cases. Unfortunately, most patients present late with metastatic disease. The prognosis is poor with a mean survival time post-operatively of 10–14 months and a 5-year survival rate of 4.5%. Although adjuvant therapy offers some loco-regional control, complete surgical resection offers the best hope for survival.
INTRODUCTION
Primary mucosal melanoma can arise anywhere along the gastrointestinal tract. In comparison with the cutaneous variant, mucosal melanoma has poorer outcomes due to late detection and high metastatic potential. The oesophagus is a rare site of origin for primary malignant melanoma with only 337 cases published in the literature [1, 2]. Here, we present two cases of metastatic primary oesophageal melanoma, which highlight the challenging nature in the management of rare but aggressive malignancy.
CASE REPORT
Case A
A 38-year-old male presented with an 8-week history of dysphagia and weight loss. He was previously well and had no relevant medical history. Clinically, he had a palpable left cervical lymph node and unremarkable dermatological and ophthalmological assessments.
His initial endoscopy showed a 12 cm fungating, pigmented tumour occupying most of lower oesophageal lumen (Fig. 1). The biopsy was highly suggestive of primary malignant melanoma. Staging computed tomography (CT) and positron emission tomography (PET) showed extensive mediastinal, left supraclavicular and coeliac lymph node enlargement (FDG avid) with no evidence of metastatic disease (Fig. 2).
An endoscopic view of the fungating melanoma involving most of the oesophageal lumen.

He was commenced on palliative radiotherapy with good symptomatic improvement. However, serial CT imaging showed interval development of metastatic lesions within the pericardial tissues, chest and liver. New metastatic nodules within the oesophagus and stomach were seen on repeat endoscopy. He was worked up for chemotherapy, however, succumbed to respiratory failure and passed away shortly before initiation of therapy.
Case B
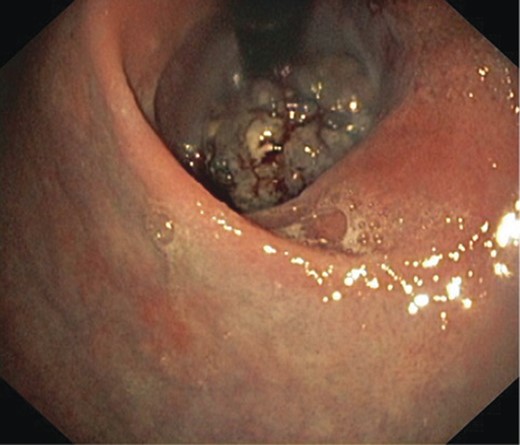
A 75-year-old male presented with a 2-month history of dysphagia, odynophagia and retrosternal post-prandial pain. He had no relevant medical history, and physical, dermatological and ophthalmological examinations proved unremarkable. Barium swallow showed filling defects in the distal oesophagus and subsequent endoscopy found an 8-cm bluish exophytic oesophageal lesion with numerous adjacent satellite lesions and moderate luminal stricturing (Fig. 3). A biopsy result indicated a poorly differentiated malignant melanoma. CT and PET showed an enlarged mediastinal node (not FDG avid) with no evidence of metastases.

An endoscopic view of the oesophageal melanoma with numerous adjacent satellite lesions.
Because of the presence of extensive satellite lesions, the patient was given a palliative course of radiotherapy, with some initial improvement. However, he rapidly re-developed worsening dysphagia, dysphonia and weight loss. An endoscopic attempt to place an oesophageal stent was aborted by intra-operative aspiration and subsequent cardiorespiratory arrest.
Disease progression was noted on repeat CT scan, showing primary lesion enlargement, extensive mediastinal lymphadenopathy with tracheal invasion and oesophageal compression. Multiple pulmonary and liver metastases were noted.
The patient and his family decided to withdraw all treatment and he was returned to his regional hospice for palliation and passed away some months later.
DISCUSSION
Primary malignant melanoma of the oesophagus is rare and accounts for 0.1–0.2% of all oesophageal malignancies. No risk factors have yet been implicated for this malignancy, although 4% of the population exhibit melanosis of the oesophagus, which may be a precursor to melanoma [3]. This malignancy tends to arise in the sixth and seventh decades with a 2:1 male-to-female preponderance [1]. In contrast to cutaneous melanoma, the oesophageal variant appears to have a higher racial predilection for the Japanese compared with Caucasians [2].
Typically, this tumour appears as a pigmented polypoid mass of a variable size in the mid- and lower third of the oesophagus, although up to a quarter of lesions can appear amelanotic [1, 4]. Where the histological diagnosis is uncertain, definitive diagnosis can made through immunomarker staining for vimentin, S-100 protein, HMB-45, Melan-A and tyrosinase [2].
The commonest symptom of primary oesophageal melanoma is dysphagia. By the time the patient is symptomatic, there is often significant tumour bulk with locally advanced, if not metastatic disease [1, 5]. Despite disease dissemination, complete surgical resection is the only treatment modality which influences survival [6]. Wide margins are advised due to the presence of satellite nodules which exist in 12% of cases [1]. Despite radical surgery, however, the prognosis is poor with a mean survival time post-operatively of 10–14 months and a 5-year survival rate of 4.5% [2]. Moreover, 77% of cases will ultimately succumb from recurrent disease within the first post-operative year [5].
The roles of adjuvant chemotherapy, radiotherapy and immunotherapy remain unclear. Although these modalities do not appear to improve survival, there may benefits in loco-regional disease control [7].
With the rarity of this aggressive disease, our understanding of the tumour biology is incomplete and there is a lack of consensus on treatment guidelines. As with other types of oesophageal cancer, patients with these tumours tend to delay seeking medical attention, by when the disease is often locally advanced and disseminated.
Early diagnosis with complete surgical resection currently offers the best hope for survival and any pigmented lesions within the oesophagus must be further investigated for malignant potential until proven otherwise.



