-
PDF
- Split View
-
Views
-
Cite
Cite
Jeyanthi N. Narayanasamy, Mohan Arunasalam Nallusamy, Nur Daliza Baharuddin, Fetus-in-fetu: a pediatric rarity, Journal of Surgical Case Reports, Volume 2014, Issue 2, February 2014, rju001, https://doi.org/10.1093/jscr/rju001
Close - Share Icon Share
Abstract
Fetus-in-fetu (FIF) is a rare entity resulting from abnormal embryogenesis in diamniotic monochorionic twins, being first described by Johann Friedrich Meckel (1800s). This occurs when a vertebrate fetus is enclosed in a normally growing fetus. Clinical manifestations vary. Detection is most often in infancy, the oldest reported age being 47. We report the case of a 4-day-old girl who was referred postnatally following a prenatal fetal scan which had revealed the presence of a multi-loculated retroperitoneal mass lesion with calcifications within. A provisional radiological diagnosis of FIF was made. Elective laparotomy revealed a well encapsulated retroperitoneal mass containing among other structures a skull vault and rudimentary limb buds. Recovery was uneventful. Here we discuss the difference between FIF and teratomas, risks of non-operative therapy and the role of serology in surveillance and detection of malignant change.
INTRODUCTION
Fetus-in-fetu (FIF) is an uncommon pathology with an incidence of 1 in 500 000 births. Less than 200 cases have been reported worldwide. Multiple theories are proposed regarding embryogenesis. One is the teratoma theory where FIF is regarded as a highly differentiated form of mature teratoma [1–3]. The other is the parasitic twin theory, according to which FIF may be a parasitic twin fetus growing within its host twin. FIF results from abnormal embryogenesis in a diamniotic monochorionic twin pregnancy. This is followed by arrest of further growth of the encased fetus due to improper blood supply or inherent defects of the encased twin.
Most FIF are anencephalic, but in almost all cases vertebral column (91%) and limb buds (82.5%) are present. During ventral folding of the trilaminar embryonic disc, one of the fetuses is enclosed in its host because of persistent anastomoses of vitelline circulation. As the superior mesenteric artery develops from the vitelline circulation, this explains its most common retroperitoneal location. Other reported sites are abdomen, scrotum, cranium, kidneys, adrenals, mediastinum and lymph nodes. A slight male preponderance has been reported. The major presenting complaint is a palpable abdominal mass. Compressive effects include jaundice, hydronephrosis, intestinal obstruction, meconium peritonitis, respiratory distress and vomiting [4–6].
CASE REPORT
We report the case of a 4-day-old baby girl with a large non-tender mass of variable consistency over the right lumbar region. Antenatal sonography during the third trimester of gestation had revealed the presence of a multilocated, cystic retroperitoneal lesion with calcification. Antenatal follow-up had otherwise been uneventful. Delivery was via Cesarean section, as there were worries of a vertex delivery resulting in obstructed labor given the fetus' distended abdomen.
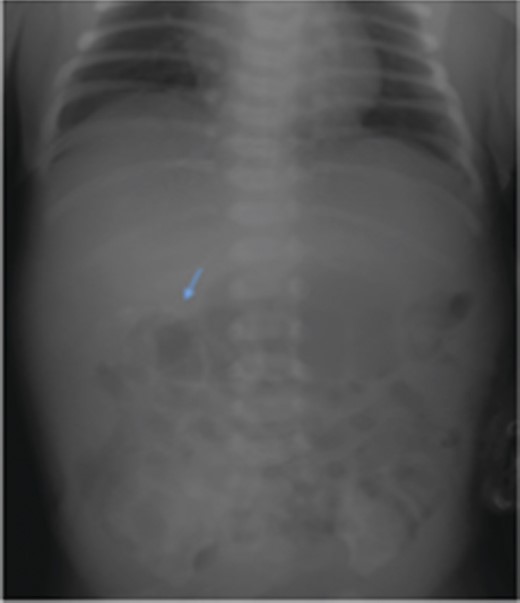
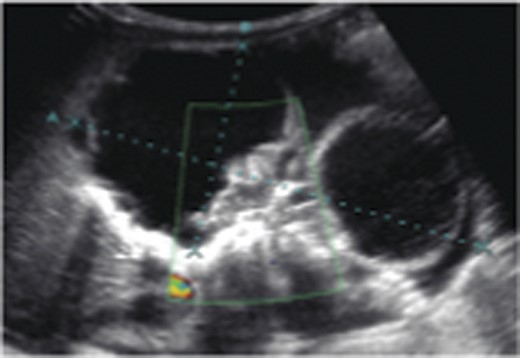
The case was referred to the Pediatric Surgery team postnatally. Birthweight was 3.6 kg. Apart from a distended abdomen, the child appeared grossly normal. Abdominal radiograph showed curvilinear calcifications over the right abdomen (Fig. 1). Ultrasonography (USG) revealed the presence of an echogenic line resembling long bones, giving rise to a provisional diagnosis of FIF (Fig. 2). An alpha feto protein (αfp) level taken at birth was markedly elevated at 13 200 IU/ml. Normal range of αfp at our center is taken to be 0–5.8 IU/ml at birth.
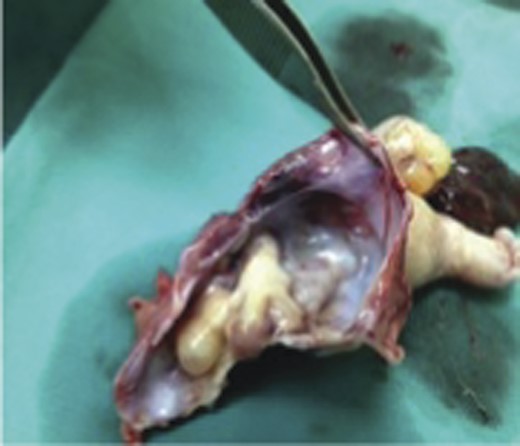
Parents were counseled for surgery. Elective laparotomy at 3 months confirmed our diagnosis. A right loin skin incision was made to allow for access into the retroperitoneal space. The well-encapsulated tumor situated anterior to the inferior vena cava was compressing the right kidney. Coronal vessels and the right ureter were located at the posterolateral aspect of tumor; these were preserved. The gross specimen measured 90 × 70 × 40 mm and was covered by a thin fibrous sac containing straw colored fluid (Fig. 3). An anencephalic fetus and limb buds could be appreciated (Figs 4 and 5).

Resected specimen seen encapsulated by a thin, intact membrane.

Rudimentary limb buds and an anencephalic fetus extracted from the sac.
The child had an uneventful recovery and was discharged home on the third postoperative day. αfp 1 month post-surgery had fallen to 387 IU/ml, levels had however normalized 3 months following surgery. Histopathological examination showed a composition of mature benign tissues. A final diagnosis of a mature cystic teratoma was made.
DISCUSSION
There is controversy as to whether FIF is a distinct entity or represents a highly organized teratoma. The main diagnostic challenge lies in differentiating this entity from an immature teratoma with its associated risk of malignancy. A teratoma is defined as a neoplasm with a slight potential for malignancy that is composed of multiple tissues foreign to the part in which they are located [7]. It is often difficult to make a distinction between teratomas and vestigial remnants that result from abortive attempts at twinning [8]. The spectrum of anomalous embryogenesis in a diamniotic monochorionic pregnancy includes conjoined symmetric twins, parasitic fetuses, embryonic vestigial fetal inclusions and organized teratoma.
A final important feature that has been used to distinguish between FIF and teratoma is the presence of a vertebral column. Willis [9] emphasized that the identification of a vertebral column secures the diagnosis of FIF and differentiates this entity from teratoma. Identification of the vertebral column indicates that fetal development of the included twin must have advanced at least to the primitive streak stage to develop a notochord, which is the precursor of the vertebral column.
Surgical excision remains the treatment of choice. Careful dissection should be done to avoid injury to surrounding structures. A case of bile duct injury has been reported. Planning of surgical access is an important preoperative consideration. The retroperitoneal approach resembling that taken in accessing the kidneys would ensure that dissection stays entirely retroperitoneal, resulting in less postoperative ileus, earlier enteral feeding and faster recovery.
Can FIF however be left alone? The presence of immature elements emphasizes the need of complete excision along with its covering membrane, as cases of malignant transformation of remnant membranes have been reported. Risks associated with FIF are hemorrhage, infection, mass effects and pleuro-peritoneal inflammation due to leak of sac contents.
Both in cases managed non-operatively and in postoperative patients, close follow-up with sonography and serology (αfp or beta-HCG levels) is recommended. Although αfp levels may be normal during the early stages of the disease, this does not preclude significant pathology. αfp is a glycoprotein molecule which has some similarities to albumin and is produced by the fetal yolk sac and liver. Its biological role is unclear but it has an important role as a diagnostic marker. Normal reference values in newborns have yet to be clearly defined [10]. A possible chance if recurrence or malignant change must be kept in mind.
Diagnosis is most often by imaging. Both magnetic resonance imaging and USG lack ionizing radiation and are ideal imaging modalities. Due to its wide availability, low cost and real-time imaging, USG has become the investigation of choice for diagnosis of fetal structures and various growth anomalies. It is the imaging modality of choice at our center.
ACKNOWLEDGEMENTS
I would like to thank Dato Mohan Nallusamy and Ms Daliza Baharuddin for all their support and guidance.
REFERENCES
- teratoma
- fetus
- infant
- laparotomy
- limb buds
- pediatrics
- retroperitoneal space
- serologic tests
- signs and symptoms
- cranium
- vertebrates
- diagnosis
- meckel's diverticulum
- prenatal care
- study of serum
- mass lesion
- surveillance, medical
- teratogenesis
- diamniotic-monochorionic twins
- malignant transformation
- fetus in fetu
- calcification



