-
PDF
- Split View
-
Views
-
Cite
Cite
Konstantinos Sapalidis, Iraklis Anastasiadis, Nicolas Panteli, Titika-Marina Strati, Lazaros Liavas, Christos Poulios, Ioannis Kanellos, Primary squamous cell carcinoma of the thyroid gland, Journal of Surgical Case Reports, Volume 2014, Issue 12, 1 December 2014, rju133, https://doi.org/10.1093/jscr/rju133
Close - Share Icon Share
Abstract
Primary squamous cell carcinoma (SCC) of the thyroid gland is a very rare entity representing <1% of all primary carcinomas of the thyroid gland with a very poor prognosis. We report a rare case of a 65-year-old woman with SCC of the thyroid gland, emphasizing the postoperative complications and poor prognosis of these patients. Surgical excision of primary SCC of the thyroid gland when possible is the optimal therapy. Chemo- and radiotherapy rarely have place in its treatment as this malignancy has a poor response to chemotherapy and in many cases is radio-resistant. Median survival of these patients is around 6 months.
INTRODUCTION
Primary squamous cell carcinoma (SCC) of the thyroid gland is a very rare entity representing <1% of all primary carcinomas of the thyroid gland [1, 2]. Only a few cases are reported in the international literature and it is described as a very aggressive tumor with a poor prognosis. Overall survival usually does not exceed 6 months after the time of diagnosis. The aim of this study is to report the case of a SCC of the thyroid gland in a 65-year-old woman, emphasizing the postoperative complications and poor prognosis of these patients.
CASE REPORT
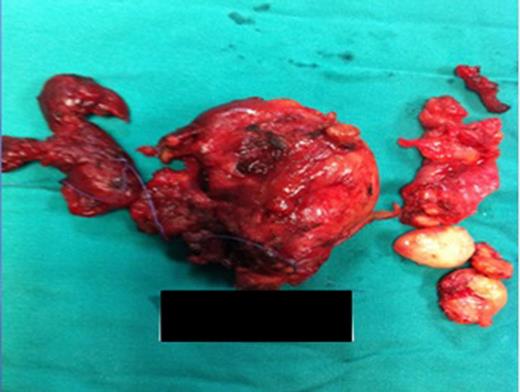
Surgical specimen: thyroid gland with an enlarged left lobe (retrosternal extension).
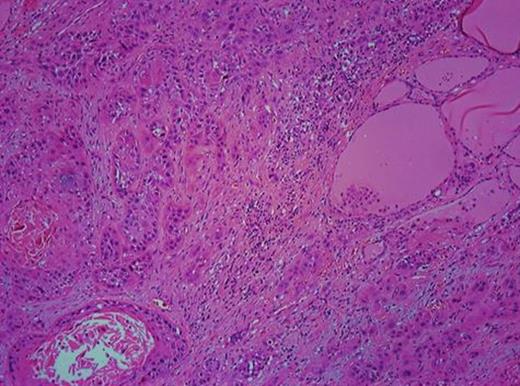
H/E ×100 section from the left lobe of the thyroid gland showing infiltrative SCC.
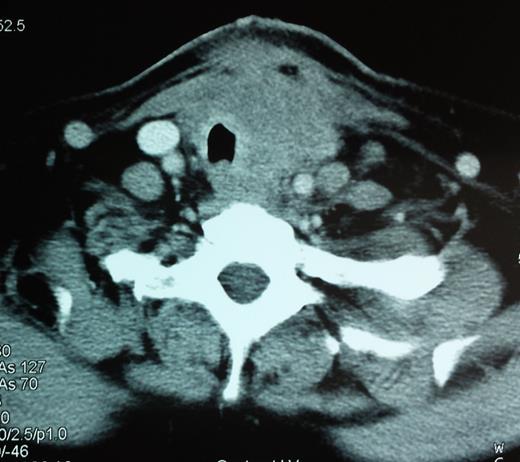
A CT scan showing a 6.2-cm mass pressuring and infiltrating the trachea and surrounding soft tissue.
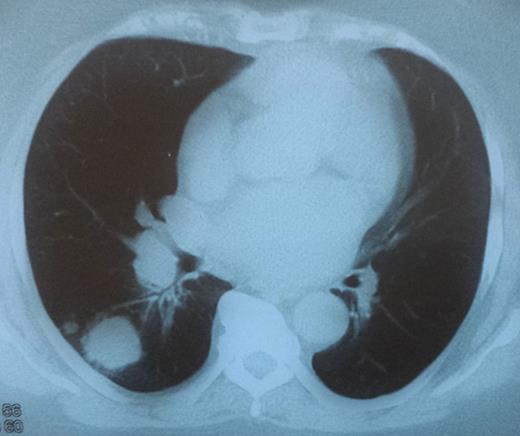
Patient was submitted to adjuvant chemotherapy as well as radiation therapy. She underwent two cycles of chemotherapy with cisplatin 70 mg/kg once a week with concomitant radiotherapy, which was abruptly terminated because of toxicity. Patient died 5 months after the surgery due to airway compromise (direct infiltration of tumor to trachea causing airway obstruction).
DISCUSSION
A primary SCC of the thyroid is rare, representing <1% of all primary thyroid carcinomas [1, 2]. Due to its rarity, only few case reports are reported in the international literature [3]. It is considered to be highly aggressive with a poor prognosis [4]. SCC affects usually older patients between the fifth and sixth decade and is usually associated with a history of goiter. In the majority of cases, the patients present at the time of diagnosis with a rapidly enlarged neck mass, followed by symptoms of infiltration and compression of adjacent neck structures (dyspnea and hoarseness). Infiltration of cervical lymph nodes may or may not be present.
Carcinoma showing thymus-like elements (CASTLE) disease of the thyroid gland, anaplastic thyroid carcinoma and metastasis from adjacent organs should be considered in the differential diagnosis. SCC is of unknown etiology, as the thyroid gland normally lacks squamous epithelium. Several theories have been suggested regarding its etiology. However, three theories have been postulated. First, the embryonic nest theory suggests that the squamous cells are derived from the remnants of thyroglossal duct or the epithelium of the thymus [5]. Secondly, the metaplasia theory suggests that these cells present as a result of environmental stimuli (inflammation and Hashimoto's thyroiditis) [6]. Thirdly, the de-differentiation theory suggests that existing papillary, follicular, medullary and anaplastic thyroid carcinoma de-differentiate into SCC [7].
Surgical excision of primary thyroid SCC with adjuvant radiotherapy and chemotherapy is the optimal treatment. However, many studies suggest that it is relatively radio-resistant and has poor response to chemotherapy [4, 8], leaving complete surgical excision the only chance of prolonging survival of these patients [9]. Patients with primary thyroid SCC have a very poor prognosis and the main cause of death is respiratory interference by direct invasion or compression of the trachea [10].
Cho et al., recently, performed a systematic review and individual participant data meta-analysis regarding primary SCC of the thyroid gland. According to this meta-analysis (89 patients), the mean age of diagnosis was 63 years (range, 24–90), a female preponderance (M : F = 1:2) was noted and the commonest complaint was the anterior neck mass. It was noted that predictability of diagnosis with fine needle aspiration cytology was accurate in less than one-third of the patients and more than half of cases had been diagnosed as papillary thyroid carcinoma or were non-diagnostic (as in our case). Complete surgical resection (Ro) of the tumor was the only significant prognostic factor in multivariable analysis, and the benefit of adjuvant treatment was not proved. Moreover, the prognosis of these patients was very poor (only 20% in 3 year survival rate) [11].
SCC of the thyroid gland is a very rare and aggressive entity with poor prognosis. Complete surgical resection (Ro) of the tumor is the only significant prognostic factor, whereas efficacy of adjuvant treatment (chemo- and radiotherapy) remains controversial in the international literature. A fatal outcome is usually a result of its complications, due to loco-regional spread of the disease to adjacent organs and structures.
CONFLICT OF INTEREST STATEMENT
None declared.



