-
PDF
- Split View
-
Views
-
Cite
Cite
Christos Konstantinidis, Panagiotis Varsos, Sotirios Kympouris, Spyridon Volteas, Migrated biliary plastic stent causing double sigmoid colon perforation, Journal of Surgical Case Reports, Volume 2014, Issue 12, 1 December 2014, rju134, https://doi.org/10.1093/jscr/rju134
Close - Share Icon Share
Abstract
A female patient was admitted to our hospital with sigmoid colon perforation caused by migrated biliary plastic stent, which was placed 2 months ago for the treatment of choledocholithiasis. The patient underwent sigmoid colon resection with primary anastomosis and was discharged on seventh postoperative day in good general condition.
INTRODUCTION
Endoscopic placement of biliary stents is performed by endoscopic retrograde cholangiopancreatography (ERCP) for the treatment of various hepatic, biliary or pancreatic lesions, either benign or malignant. Two categories of material are used: plastic and metallic stents. Nowadays, stenting of the biliary duct is a commonly used procedure, amenable to early or late complications. Stent migration is among them, which usually causes no significant problems. Distal (intestinal and colonic) migration is less usual than proximal (duodenal). Generally, in order to prevent migration, stent should be placed across the sphincter of Oddi and removed or changed in 3–6 months. If migration of biliary stent occurs, it usually passes in the feces or remains in the bowel causing no symptoms. In rare cases, biliary stents cannot pass through the bowel and colonic perforation can occur. In such case, urgent surgical intervention is required. The options of surgical procedure depend on findings at laparotomy.
CASE REPORT

A CT scan showing the upper edge of the biliary stent perforating the antimesenteric surface of the sigmoid colon (red arrow).

A CT view of the same patient showing the lower edge of the biliary stent perforating the sigmoid colon (red arrow).
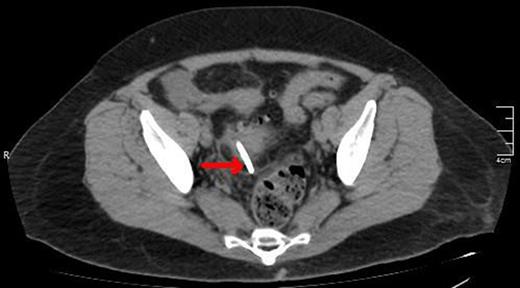
A lower CT view of the same patient showing the stent (red arrow).
DISCUSSION
In the literature, the reported incidence of biliary stent migration is ∼10% of cases, with plastic stents migrating more often than metallic stents [1, 2]. Stents migrate most often to the duodenum and rarely cause complications of the colon [3]. Gut perforation occurs in less than 1% of biliary stent migrations, as an early or late consequence [4–6]. Patients who suffer more are those with diverticular disease, hernia or intra-abdominal adhesions. Diagnosis of migrated biliary stent necessitates its immediate removal [7]. In cases of intestinal perforation, exploratory laparotomy is indicated with stent removal and abdominal lavage. Further surgical intervention includes resection of the affected bowel with Hartmann's procedure or primary anastomosis, depending on the contamination of the surgical field.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
Author notes
†All authors equally contributed to this work.



