-
PDF
- Split View
-
Views
-
Cite
Cite
Sebastien Crosswell, Shin-Jae Rhee, Wolfgang W. Wagner, Unusual fracture combination in a paediatric acute ankle (combined medial talar compression fracture with medial malleolus fracture in an immature skeleton): a case report, Journal of Surgical Case Reports, Volume 2014, Issue 10, October 2014, rju100, https://doi.org/10.1093/jscr/rju100
Close - Share Icon Share
Abstract
Talar compression fractures are uncommon orthopaedic injuries, especially in the immature skeleton. Fractures of the talar body constitute >5% of all foot and ankle fractures. The combination of a medial compression fracture and corresponding medial malleolar fracture is rare and not previously reported injury in the literature. We present a case report of a skeletally immature 15-year-old Caucasian male who sustained a medial malleolar and corresponding medial talus fracture after being ejected from his pushbike. This report outlines the potential difficulties in diagnosing an unusual fracture combination and the importance of initial management including necessary diagnostic imaging to identify such injuries. Through this case, we aim to highlight the need for having high suspicions of underlying fractures in paediatric trauma cases. The long-term complications and risks of osteonecrosis of the talus can have detrimental effect on a patient's outcome; therefore, we also emphasize the need for regular monitoring and long-term follow-up.
INTRODUCTION
Fractures of the talus occur infrequently, often reported to be involving the talar neck, and are associated with high-energy trauma. Fractures involving the talar body have only been reported infrequently in the literature, and more specifically, compression fractures of the body constitute ∼3% of all adult foot and ankle fractures [1]. Such injuries usually occur in the adult population, and occur with significant soft tissue damage, frequently resulting in post-traumatic osteoarthritis of the ankle and subtalar joint. Although fractures of the medial malleolus are common lower limb injuries, the combination of talar body compression fracture and medial malleolus fractures that occurred in this case has never been reported in the literature. The purpose of this case report is to consider these particular fractures as a possible differential diagnosis in skeletally immature patients who sustain lower limb trauma, even when there is no definitive evidence on initial plain radiographs.
CASE REPORT
An otherwise fit and well 15-year-old Caucasian male patient, who was cycling down a hill, collided with an obstacle after being ejected over the handlebars of his pushbike. In the Emergency Department, the patient was appropriately triaged according to ATLS protocol which identified isolated closed injuries to his clavicle, and bilateral lower limbs, with no neurovascular compromise [2]. No head or neck injuries were sustained and a secondary survey revealed no other injuries other than some superficial abrasions. Plain radiographs revealed a left undisplaced clavicle fracture, an angulated extra-articular fracture of the left distal tibia and a right ankle talar tilt with no evidence of any bony fracture (Fig. 1). Initial management in the Emergency department included analgesia administration, a collar and cuff for his clavicle fracture and below knee plaster of Paris (POP) backslab for his bilateral lower limb injuries, with strict elevation and neurovascular monitor.

Right ankle plain radiograph demonstrating talar tilt and increased medial tibio-talar joint space.
The patient subsequently underwent a manipulation under anaesthesia and POP application of his left distal tibia and right ankle to correct the talar displacement. Despite this, post-operative radiographs of the right ankle showed persistent widened medial tibio-talar joint, and the patient developed considerable right ankle pain and soft tissue swelling which did not correspond with the initial radiograph findings. Magnetic resonance imaging (MRI) of the right ankle joint was performed which revealed extensive marrow oedema through the medial malleolus epiphysis and the medial body of the talus. There was evidence of disruption of the medial cortex of the talus which explained the widened medial tibio-talar joint (Fig. 2). No disruptions of the epiphyseal plates or ligamentous structures were identified. The injury around the tibio-talar joint was identified as an undisplaced fracture through the postero-medial talus with a corresponding ‘kissing’-type lesion of the inner surface of the medial malleolus with gross soft tissue oedema. In view of the overlooked skeletal injury, a further computer tomography (CT) scan of the ankle joint was performed which confirmed a fragmented undisplaced fracture of the postero-medial aspect of the talus, with the anterior subtalar joint remaining intact and an undisplaced fracture through the medial malleolus (Fig. 3).
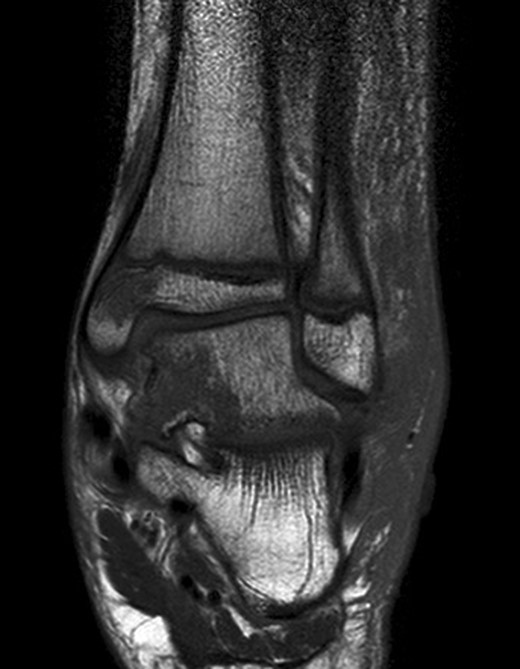
Right ankle MRI coronal view demonstrating bone marrow oedema in the medial malleolus and medial body of talus.
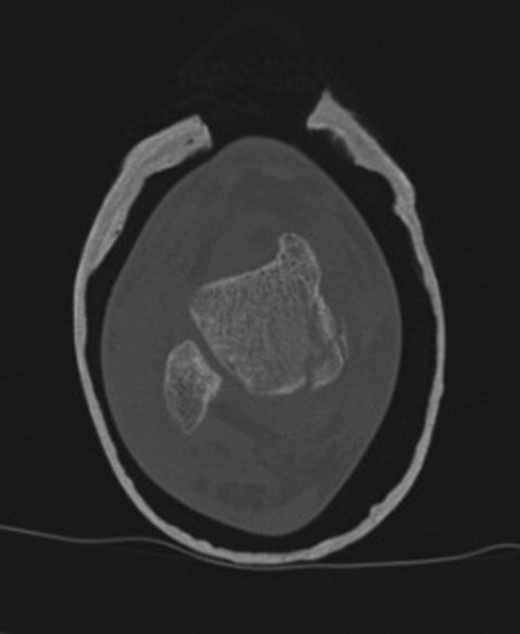
Right ankle CT axial view demonstrates undisplaced compression fracture of the medial body of the talus.
With patient and family involvement from the outset, and special input from the regional paediatric orthopaedic team, it was decided that the undisplaced nature of the fracture would be amenable to non-operative management. The right ankle was treated in a below knee moulded POP cast, with 6 weeks non-weight bearing status. The patient was followed up with radiographs on a weekly basis for the first 3 weeks, and at 6 weeks, radiographs did not show evidence of further displacement of the talus or early signs of radiological osteonecrosis [3].
At 12 weeks follow-up, the patient was weight bearing comfortably with near full range of movement. A repeat CT and MRI scan showed no evidence of displacement of the fracture fragments with good evidence of talus fracture healing. MRI revealed reduction in bone marrow signal changes with no evidence of subchondral collapse (Figs 4 and 5).

12-week follow-up MRI scan confirms reduction in bone marrow oedema in injured medial tibio-talar joint.
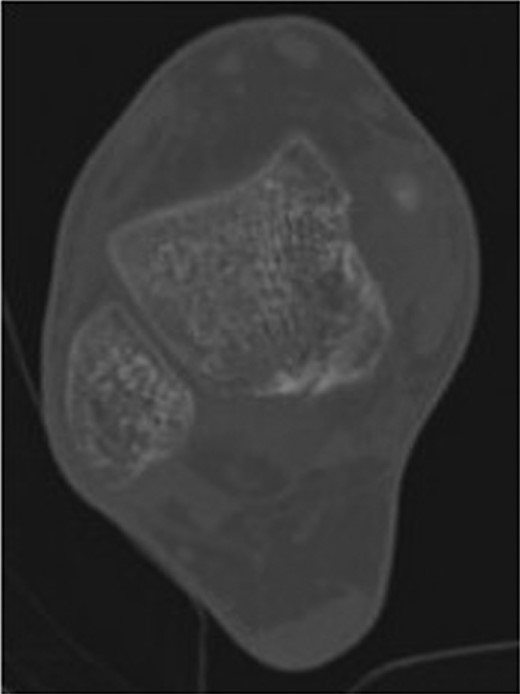
12-week follow-up CT axial view of the talus confirms no further displacement of the fracture nor any evidence of osteonecrosis. There is radiological evidence of callus bridging the fracture site.
At 12-month follow-up, the patient was not experiencing any pain from either legs and did not complain of any swelling. On examination, there was no swelling around the right foot/ankle and had full range of movement in the ankle joint. The patient was happy to fully weight bear and had engaged in normal sporting activities.
DISCUSSION
Fractures of the talus are rare constituting >5% of all foot injuries and body fractures comprise >1% of all talus fractures [1]. In the paediatric age group, the combination of fractures seen in this case are even less common, with no records in the literature to the best of our knowledge. Byrne et al. have previously reported a talar neck fracture in a skeletally immature patient, where the injury was not fully appreciated on plain radiograph. The case report again highlights the rarity of this type of fracture in the paediatric age group and advocates the need for CT scan to correctly identify these injuries. Furthermore, they emphasize the risk of osteonecrosis, arthrosis, delayed union, neuropraxia and the need for long-term follow-up [4].
Ankle injuries in this age group often leave ligaments intact and cause bony injury. If the bony structures are involved, they tend to be bone bruises which are missed on the plain radiographs. Launay et al. [5] describe 6% of their 116 acute paediatric ankle injuries as fractures which were only evident on MRI. These injuries were all localized to the lateral aspect of the ankle, unlike our case report involving the medial ankle. Furthermore, an MRI study by Endele et al. [6] confirmed that all of their paediatric acute ankle cases demonstrated bone bruising on MRI, with 10% of their cases involving bony fractures. These bony injuries were all bony avulsions. Our case study therefore highlights a very underdiagnosed acute ankle injury in a paediatric patient, with a compression fracture of the talar body and associated medial malleolar fracture.
Peripheral fractures of the talus bone are uncommon and often overlooked on initial investigations. Boack and Manegold [7] advocate the need for CT scanning as the imaging modality of choice and its importance for decision making on treatment. The outcome is related to the degree of the chondral lesion and the degree of instability of the subtalar joint, but it may be poor due to the choice of treatment, whether it be conservative or surgical [7]. Early diagnosis and proper treatment achieve the best possible results and reduces the risk of non-union and malalignment with slight subtalar instability or osseous overgrowth with secondary impingement and post-traumatic subtalar arthritis [7].
In a 15-year-old boy this would have a detrimental effect on the patient quality of life and functional ability in the future. Early CT scans can more accurately assess the severity of the talar fracture and offers the best information for an appropriate treatment plan [8]. In the case described above, MRI and CT scans were performed; however, diagnosis could have been formulated from either modality and clinical examination to reveal the talar fracture not clearly seen on plain radiographs. The choice of MRI modality is exemplified by Launay et al. [5] who demonstrated ∼40% of acute paediatric ankle injuries were identified as bony only on MRI. Furthermore, Abraham et al. [9] reported two case reports of non-displaced shear fractures of the talar body that were not identified initially and recommended that talar body fractures should be considered in patients with an axial loading injury mechanism and diffuse ankle soft tissue swelling, when no other fracture is identified on plain radiographs. It is therefore important to highlight through this case study the importance of early CT or MRI imaging if no fracture is seen on plain radiographs but significant soft tissue injury is seen.
In this case report, close monitoring of the patient was required to firstly monitor that there was no displacement of fragments and secondly to monitor for clinical or radiological signs of non-union or avascular necrosis. Vallier et al. [10] showed that despite early surgery in displaced talar body fractures, early complications are not infrequent and most patients develop radiographic evidence of osteonecrosis and/or post-traumatic arthritis. In contrast, Eberl et al. [11] observed no persistent osteonecrosis in patients younger than 12 years with talus fractures, and reported favourable outcomes in the majority of cases irrespective of the mode of treatment. Jensen et al. [12] also report an excellent long-term prognosis of minimally displaced and undisplaced fractures of the talus in the paediatric population. In this case, due to the undisplaced nature of the fracture, a good outcome was expected.
Talar body fractures of this nature are very uncommon and in paediatric patients even more unusual. This case report outlines the importance of having a high suspicion of unusual bony injury in paediatric trauma patients, and early diagnosis of these fractures using MRI or CT imaging, as they can be overlooked on plain radiographs. Strict regular follow-up is required to monitor the risk of non-union and avascular necrosis. We advocate close weekly monitoring for the first 6 weeks with follow-up CT or MRI to confirm consolidation and improvement in bone marrow oedema.
Written informed consent was obtained from the patient and parents for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
AUTHORS' CONTRIBUTIONS
All authors involved in the treatment and interpretation of the patient injury and literature research. S.C. and S.J.R. were major contributors in writing the manuscript. All authors read and approved the final manuscript.



