-
PDF
- Split View
-
Views
-
Cite
Cite
Ryan P.C. Higgin, Michael A. Glaysher, Bashir A. Zeidan, Andrew J.G. Miles, Complexities of abdominoperineal surgery: synchronous resection of an ano-rectal adenocarcinoma and pelvic schwannoma, Journal of Surgical Case Reports, Volume 2014, Issue 1, January 2014, rjt120, https://doi.org/10.1093/jscr/rjt120
Close - Share Icon Share
Abstract
Abdominoperineal resection (APR) is indicated for low rectal/ano-rectal cancers. It necessitates fastidious pelvic dissection posing certain operative difficulties. We present the surgical challenges in a unique case of a patient presenting with a low rectal adenocarcinoma and a synchronous pelvic schwannomas, both requiring resection. A 71-year-old gentleman presented for surveillance colonoscopy following previous excision of colonic polyps. This investigation revealed a polypoid mass at the ano-rectal junction which was histologically proven as an adenocarcinoma with high-grade dysplasia. A staging computed tomography scan revealed an incidental 10 × 15 cm homogeneous, pre-sacral mass. After meticulous operative planning, the patient underwent successful open resection of this mass and concurrent APR for his low rectal lesion. This case demonstrates a rare presentation of a low rectal adenocarcinoma and concurrent pelvic schwannoma. We discuss the technical difficulties encountered in the management of such complex pelvic tumours and highlight the successful outcomes of the synchronous resection.
INTRODUCTION
Colorectal cancer is a common malignant disease affecting a significant proportion of both the population in the UK and worldwide. Adenocarcinoma accounts for 95% of histological tissue diagnoses. The National Health Service Bowel Cancer Screening Programme (BCSP) has been developed to screen the UK population starting from the age of 60–69 years [1, 2].
A schwannoma is a benign tumour of Schwann cells arising from a nerve sheath. It is an uncommon tumour largely associated with neurofiromatosis or a vestibular neuroma. This tumour is rarely identified within the pelvic cavity (07–2.7%) [10].
CASE REPORT
A 71-year-old asymptomatic gentleman with known history of colonic polyps underwent a follow-up surveillance colonoscopy through the BCSP. He had a background of type 2 diabetes mellitus, ischaemic heart disease and diverticular disease. Colonoscopy revealed a 1-cm firm polypoid mass at the ano-rectal junction (Fig. 1). Subsequent endoscopic mucosal resection was performed and the tissue was sent for histological analysis. This confirmed a tubulo-villous adenocarcinoma. As per national guidelines the patient underwent a staging computed tomography (CT) scan. This revealed a 10 × 15 cm homogenous mass arising from within the pelvis (Fig. 2). The mass appeared to be continuous with a neural foramen arising from the sacrum. Further imaging confirmed the mass extending into sacral segment S1 inferiorly, lumbar segments L4 superiorly and the bladder anteriorly. A regional multidisciplinary team discussion concluded that abdominoperineal resection (APR) was the most appropriate surgical approach for removal of both pathologies in their entirety.
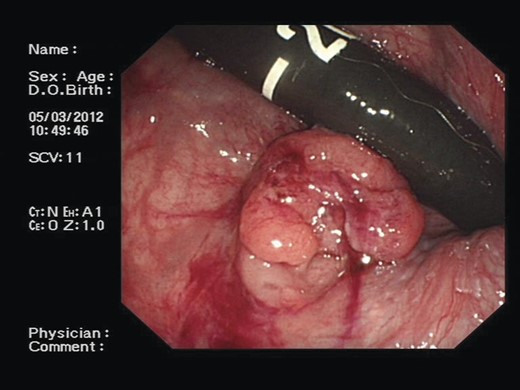
A colonoscopic image demonstrating ∼1-cm polypoid mass at the ano-rectal junction.
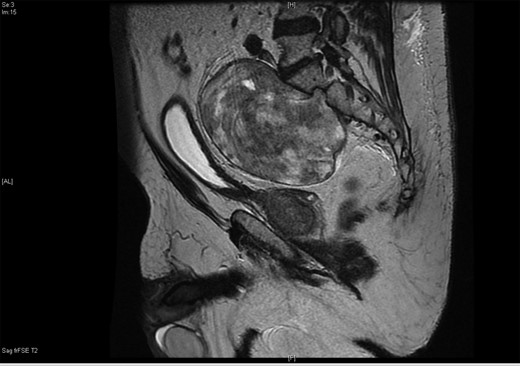
The 10 × 15 cm pre-sacral pelvic mass on sagittal contrast CT.
Within weeks the standard approach to an open APR was commenced.
The upper and mid-rectum were successfully mobilized from anterior to posterior behind the seminal vesicles using circumferential dissection techniques. Full rectal mobilization was made complex by the large 10 × 15 cm pre-sacral mass obstructing dissection planes down to the pelvic floor posteriorly. The sigmoid colon was subsequently divided ∼15 cm above the peritoneal reflection and retracted anteriorly to allow access to the tumour (Fig. 3).

On approaching the mass the pre-sacral fascia was opened to the left side of the midline to gain entry to the tumour pseudocapsule. Upon dissection copious bleeding arose from the common iliac vein to which the tumour was adherent. Intra-operative cell salvage was then commenced and haemostasis was achieved with direct pressure and vascular repair with a 4.0-polypropylene suture. The schwannoma was then fully mobilized from its anterior and lateral fascial attachments leaving it attached to the sacrum posteriorly. Lastly, the tumour was separated from the sacrum. Pre-sacral venous bleeding was packed before complex suture ligation and diathermy of disrupted veins achieved haemostasis. The estimated blood loss was ∼1600 ml and this was replaced with 1000-ml cell salvage product together with one unit of cross-matched red cells.
The perineal dissection was then completed and an end colostomy fashioned in the left iliac fossa. The abdominal wound was closed en-mass with clips to the skin. The patients' post-operative haemoglobin was 114 g/l. The patient was discharged home 9 days post-operation and remained very well at his 3-month outpatient follow-up. Pathology reports confirmed removal of a pT1N0M0 adenocarcinoma with clear margins in addition to a benign schwannoma.
DISCUSSION
Colon cancer is prevalent within the UK population. It encompasses ∼13% of all cancer diagnoses in both sexes and both prevalence and mortality are projected to increase alongside the ageing population [3]. With the introduction of the BCSP the diagnosis and management of bowel cancer has never been more successful [4]. Adenocarcinoma is the most frequently identified subtype of colorectal malignancy comprising over 95% of all histological diagnoses. The locality of colorectal adenocarcinomas is approximated to be two-thirds of colonic and one-third of rectum and anus [2]. Cancers located within the rectum are divided by location into the upper, mid- or lower rectum and anus. In this instance both the locality and stage of the tumour dictate the preferred surgical approach.
Two principal approaches are exercised for removal of ano-rectal disease: anterior resection (AR) or APR. Sparing the anal sphincter, the AR is the preferred approach for disease; however, an APR is required for rectal cancers arising low in the rectum where tumour clearance sacrifices the sphincter complex. In this case the pT1 tumour was involving the anal canal and required an APR.
The APR, also known as ‘Miles’ Operation', was first described by (William) Ernest Miles in his Lancet publication in 1908 [5]. It was Miles who first established the necessity of tissue and organ excision in relation to lymphatic spread of malignant ano-rectal disease. Miles' operation remains to be the basis of modern surgical approaches to lower ano-rectal cancer.
Complications following APR are common and have a known association with decreased quality of life of patients compared with the AR. Such complications include perineal wound breakdown, abscess formation and the development of sinus tracts. These all have a strong association with pre-operative co-morbidities and the extent of tumour invasion [6]. Such co-morbidities include diabetes mellitus, smoking and cardio-respiratory disease [7]. Diabetes mellitus has been show to directly impact the rate of perineal wound healing and associated with wound breakdown [8].
A schwannoma is a rare tumour consisting of Schwann cells arising from a nerve sheath. Aside from cranial nerves I and II, which do not possess Schwann cells, schwannomas can arise from any nerve sheath. Though largely benign, an ∼1% of cases are reported to be malignant in the form of a neurofibrosarcoma [9]. The incidence of those arising within the retroperitoneum is low (0.7–2.7%) [10]. Retroperitoneal schwannomas are often found incidentally during abdominal examination or imaging. As the tumour is habitually benign symptoms arise when the tumour exerts mass or pressure effects on surrounding tissues and organs. With a tumour likely to continue to enlarge, resulting in pressure symptoms, complete surgical resection is considered curative.
In our case we report the successful outcome following the exceptionally rare discovery of these two concurrent pelvic tumours. Key aspects to the success of this case were anticipating blood loss, utilizing intra-operative cell salvage and modifying the approach to the traditional APR.



