-
PDF
- Split View
-
Views
-
Cite
Cite
Yutaka Shimada, Tomoyuki Okumura, Shozo Hojo, Kenta Sukegawa, Takuya Nagata, Shinichi Hayashi, Kazuhiro Tsukada, Synchronous asymptomatic colonic metastasis from primary esophageal squamous cell carcinoma, Journal of Surgical Case Reports, Volume 2014, Issue 1, January 2014, rjt117, https://doi.org/10.1093/jscr/rjt117
Close - Share Icon Share
Abstract
The management of synchronous asymptomatic colonic metastases from primary esophageal squamous cell carcinoma (ESCC) has not yet been reported. A 64-year-old male patient was diagnosed with middle thoracic ESCC. The patient received chemoradiotherapy and incomplete response/stable disease was achieved. Preoperative colonoscopy revealed a 1.0-cm submucosal tumor at the splenic flexure of the colon, and biopsy results indicated possible metastasis from primary ESCC. The patient underwent subtotal esophagectomy and the colonic tumor was excised. A postoperative pathological diagnosis confirmed that the colonic tumor had metastasized from primary ESCC. Even though the patient was discharged 18 days after surgery without any complications, he died on the 72nd postoperative day due to multiple bone metastases and pleural dissemination. Our findings suggest that even with well-controlled and asymptomatic colonic metastasis from primary esophageal lesions, the prognosis of patients with primary ESCC is poor.
INTRODUCTION
Hematogenic metastasis from primary esophageal squamous cell carcinoma (ESCC) commonly occurs in the lungs, liver and bones. Metastasis to the gastrointestinal tract from primary ESCC is rare, with gastric wall metastasis being the most frequently observed followed by metastasis to the small intestine. However, colonic metastasis is very rare, and has only been described in two English studies.
Colonic metastasis from primary ESCC is regarded as distant metastasis. Operative indication for colonic metastasis exists for colonic obstruction or accidental detection during surgery. However, the management of synchronous asymptomatic colonic metastasis from primary ESCC had not yet been reported. We here describe the simultaneous resection of primary ESCC and colonic metastasis.
CASE REPORT
A 64-year-old male consulted one of our hospitals due to progressive dysphagia in August 2012. An endoscopic examination revealed middle thoracic ESCC (Fig. 1). Computed tomography (CT) scans showed possible invasion of the aorta and multiple lymph node metastases (T4bN3M1 stage4) (Fig. 1). The length of the tumor was ∼10 cm on CT scans. The patient received definitive chemoradiotherapy [two courses of cisplatin and 5-fluorouracil (FP) plus 50.4 Gy] followed by one course of FP chemotherapy, and incomplete response/stable disease was achieved. Although an endoscopic biopsy specimen was positive for cancer (Fig. 1), post-treatment CT showed no invasion of the aorta. Fluorine-18-fluorodeoxyglucose positron emission tomography (FDG-PET) also suggested that the size of the tumor was diminished. The patient underwent colonoscopy to prepare for colonic interposition because the radiation field included the upper part of the stomach. Preoperative colonoscopy revealed a 1.0-cm submucosal tumor at the splenic flexure, and biopsy results indicated possible metastasis from primary ESCC (Fig. 2). The submucosal lesion was positive for cytokeratin 5/6 (CK5/6), CK14 and p63, and negative for CK20 and Caudal type homeobox 2 (CDX2) (Fig. 2). Colonic metastasis was not detected by FDG-PET before or after chemoradiotherapy. No other obvious hematogenic metastases were noted after chemoradiotherapy.
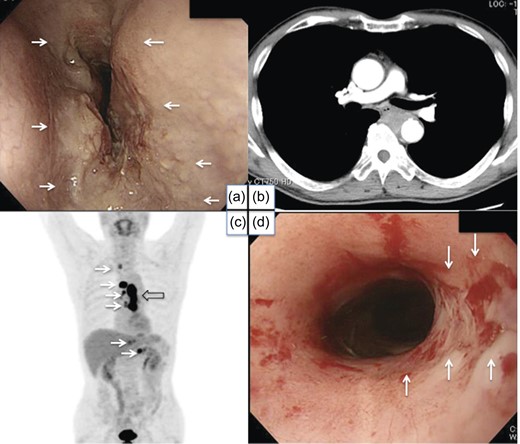
Pretreatment endoscopic examination, CT scan, FDG-PET and post-treatment endoscopic examination. A tumor was found in the middle thoracic esophagus (a). CT scans revealed possible invasion of the aorta (b) and multiple lymph node metastases. FDG-PET also suggested the spread of tumors (open arrow) and multiple lymph node metastases (white arrows) (c). Post-treatment endoscopy showed a marked reduction in the size of the tumor, while residual carcinoma cells were detected in a biopsy specimen (white arrows) (d).
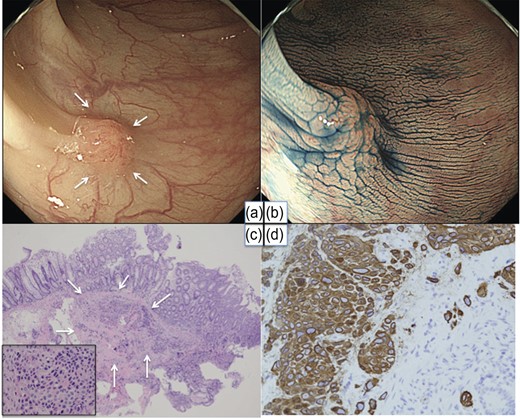
Colonoscopy and histology of a biopsy specimen. A small elevated lesion was found at the site of the splenic flexure (white arrows) (a and b). Hematoxylin–eosin staining and CK14 staining (c and d).
The patient underwent subtotal esophagectomy by right thoracotomy with thoraco-abdominal lymph node dissection and reconstruction with a gastric tube in January 2013. Local excision of the colonic submucosal tumor was also performed (Fig. 3). A postoperative pathological diagnosis revealed that the colonic tumor metastasized from primary ESCC and remnant viable carcinoma cells were found in the primary site of the esophagus and lymph nodes (Fig. 3). Even though the patient was discharged 18 days after surgery without any complications, he died on the 72nd postoperative day due to multiple bone metastases and pleural dissemination.
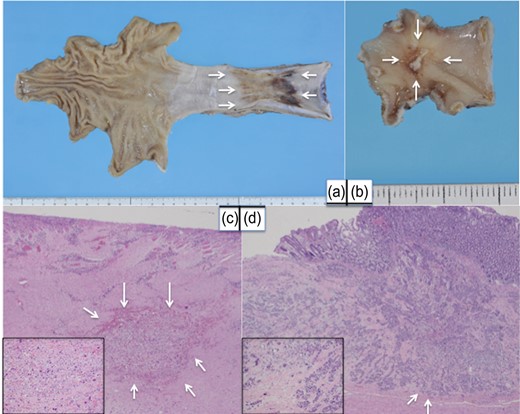
Macroscopic and microscopic findings of resected esophagus and colon. A flat tumor was found in the esophagus (white arrows) (a). A 1.0-cm submucosalcolonic tumor was excised (white arrows) (b). Remnant viable cells were observed in the esophagus (white arrows) and lymph nodes (c). Colonic metastasis was located in the submucosa and slight invasion of the muscularispropria was observed (white arrows) (d).
DISCUSSION
Metastatic tumors from extra-abdominal sites are rarely observed in the gastrointestinal tract. Colonic metastasis from primary ESCC is very rare, and has only been described in two English studies and one Japanese study [1–3]. There have also been six Japanese meeting abstracts (Table 1).
Characteristics of patients with colonic metastasis from primary ESCC (including meeting abstracts)
| Case no. . | Age and sex . | Location of colonic metastasis . | Symptoms of colonic metastasis . | Treatment for colonic metastasis . | Interval from the initial treatment of ESCC . | Location of primary ESCC . | Histology of ESCC . | Treatment for ESCC and other metastases . | Prognosis . | Author . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 50, M | TC, DC | Detection of a tumor mass | Left hemicolectomy | Metachronous (1Y2M after the first OP) | Lt, Mt | Mod | SE. 8M after SE, CRT for cervical LN metastasis | 5M died | Maruyama et al. [1] |
| 2 | 56, M | DC | Ileus | Left hemicolectomy | Metachronous (9M after the first OP) | Lt | Wel | SE followed by FP and 50 Gy | 9M died | Totsuka et al. (1998) (PJM) |
| 3 | 56, M | TC | Intraoperative detection | Partial resection of the colon | Synchronous | LtAe | Mod | SE followed by FP | 2M died | Shinohara et al. (2000) (PJM) |
| 4 | 70, F | TC-DC | Ileus | Left hemicolectomy | Metachronous (2Y2M after the first OP) | Mt | Mod | SE followed by 45 Gy | Unknown | Horikawa et al. (2001) (PJM) |
| 5 | 74, M | S | Ileus | Hartmann OP | Metachronous (2Y11M after the first OP) | Ae | Mod | SE. 2Y11M after SE, liver metastasis | Unknown | Mizutani et al. (2008) (PJM) |
| 6 | 73, M | S | Ileus | Hartmann OP | Metachronous (1Y after the first OP) | Lt | Por | SE. 11M after SE, CRT for metastasis to the gastric tube | 14M died | Ogaki et al. (2008) (PJM) |
| 7 | 59, F | Ce | Dermatomyositis | Ileocecal resection | Metachronous (1Y after the first OP) | Mt | SCC | SE followed by FP | Unknown | Yamamoto et al. (2009) (PJM) |
| 8 | 60, M | TC | Intraoperative detection | Segmental resection of the colon | Synchronous | Mt | Mod | CRT for ESCC. Local excision of gastric metastasis | Unknown | Karwasra et al. [2] |
| 9 | 51, M | S | Bloody stools | Chemotherapy | Synchronous | MtLtAe | Mod | CRT | 1Y alive | Iwase et al. [3] |
| 10 | 64, M | TC-DC | Asymptomatic | Partial resection of the colon | Synchronous | Mt | Por | CRT and SE | 2.5M died | Our case |
| Case no. . | Age and sex . | Location of colonic metastasis . | Symptoms of colonic metastasis . | Treatment for colonic metastasis . | Interval from the initial treatment of ESCC . | Location of primary ESCC . | Histology of ESCC . | Treatment for ESCC and other metastases . | Prognosis . | Author . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 50, M | TC, DC | Detection of a tumor mass | Left hemicolectomy | Metachronous (1Y2M after the first OP) | Lt, Mt | Mod | SE. 8M after SE, CRT for cervical LN metastasis | 5M died | Maruyama et al. [1] |
| 2 | 56, M | DC | Ileus | Left hemicolectomy | Metachronous (9M after the first OP) | Lt | Wel | SE followed by FP and 50 Gy | 9M died | Totsuka et al. (1998) (PJM) |
| 3 | 56, M | TC | Intraoperative detection | Partial resection of the colon | Synchronous | LtAe | Mod | SE followed by FP | 2M died | Shinohara et al. (2000) (PJM) |
| 4 | 70, F | TC-DC | Ileus | Left hemicolectomy | Metachronous (2Y2M after the first OP) | Mt | Mod | SE followed by 45 Gy | Unknown | Horikawa et al. (2001) (PJM) |
| 5 | 74, M | S | Ileus | Hartmann OP | Metachronous (2Y11M after the first OP) | Ae | Mod | SE. 2Y11M after SE, liver metastasis | Unknown | Mizutani et al. (2008) (PJM) |
| 6 | 73, M | S | Ileus | Hartmann OP | Metachronous (1Y after the first OP) | Lt | Por | SE. 11M after SE, CRT for metastasis to the gastric tube | 14M died | Ogaki et al. (2008) (PJM) |
| 7 | 59, F | Ce | Dermatomyositis | Ileocecal resection | Metachronous (1Y after the first OP) | Mt | SCC | SE followed by FP | Unknown | Yamamoto et al. (2009) (PJM) |
| 8 | 60, M | TC | Intraoperative detection | Segmental resection of the colon | Synchronous | Mt | Mod | CRT for ESCC. Local excision of gastric metastasis | Unknown | Karwasra et al. [2] |
| 9 | 51, M | S | Bloody stools | Chemotherapy | Synchronous | MtLtAe | Mod | CRT | 1Y alive | Iwase et al. [3] |
| 10 | 64, M | TC-DC | Asymptomatic | Partial resection of the colon | Synchronous | Mt | Por | CRT and SE | 2.5M died | Our case |
AC, ascending colon; TC, transverse colon; DC, descending colon; Ce, cecum; S, sigmoid colon; Ut, upper thoracic esophagus; Mt, middle thoracic esophagus; Lt, lower thoracic esophagus; Ae, abdominal esophagus; Wel, well-differentiated squamous cell carcinoma; Mod, moderately differentiated squamous cell carcinoma; Por, poorly differentiated squamous cell carcinoma; SCC, squamous cell carcinoma; LN, lymph node; SE, subtotal esophagectomy; FP, fluorouracil and cisplatin; OP, operation; CRT, chemoradiation; PJM, Proceedings of Japanese Meetings.
Characteristics of patients with colonic metastasis from primary ESCC (including meeting abstracts)
| Case no. . | Age and sex . | Location of colonic metastasis . | Symptoms of colonic metastasis . | Treatment for colonic metastasis . | Interval from the initial treatment of ESCC . | Location of primary ESCC . | Histology of ESCC . | Treatment for ESCC and other metastases . | Prognosis . | Author . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 50, M | TC, DC | Detection of a tumor mass | Left hemicolectomy | Metachronous (1Y2M after the first OP) | Lt, Mt | Mod | SE. 8M after SE, CRT for cervical LN metastasis | 5M died | Maruyama et al. [1] |
| 2 | 56, M | DC | Ileus | Left hemicolectomy | Metachronous (9M after the first OP) | Lt | Wel | SE followed by FP and 50 Gy | 9M died | Totsuka et al. (1998) (PJM) |
| 3 | 56, M | TC | Intraoperative detection | Partial resection of the colon | Synchronous | LtAe | Mod | SE followed by FP | 2M died | Shinohara et al. (2000) (PJM) |
| 4 | 70, F | TC-DC | Ileus | Left hemicolectomy | Metachronous (2Y2M after the first OP) | Mt | Mod | SE followed by 45 Gy | Unknown | Horikawa et al. (2001) (PJM) |
| 5 | 74, M | S | Ileus | Hartmann OP | Metachronous (2Y11M after the first OP) | Ae | Mod | SE. 2Y11M after SE, liver metastasis | Unknown | Mizutani et al. (2008) (PJM) |
| 6 | 73, M | S | Ileus | Hartmann OP | Metachronous (1Y after the first OP) | Lt | Por | SE. 11M after SE, CRT for metastasis to the gastric tube | 14M died | Ogaki et al. (2008) (PJM) |
| 7 | 59, F | Ce | Dermatomyositis | Ileocecal resection | Metachronous (1Y after the first OP) | Mt | SCC | SE followed by FP | Unknown | Yamamoto et al. (2009) (PJM) |
| 8 | 60, M | TC | Intraoperative detection | Segmental resection of the colon | Synchronous | Mt | Mod | CRT for ESCC. Local excision of gastric metastasis | Unknown | Karwasra et al. [2] |
| 9 | 51, M | S | Bloody stools | Chemotherapy | Synchronous | MtLtAe | Mod | CRT | 1Y alive | Iwase et al. [3] |
| 10 | 64, M | TC-DC | Asymptomatic | Partial resection of the colon | Synchronous | Mt | Por | CRT and SE | 2.5M died | Our case |
| Case no. . | Age and sex . | Location of colonic metastasis . | Symptoms of colonic metastasis . | Treatment for colonic metastasis . | Interval from the initial treatment of ESCC . | Location of primary ESCC . | Histology of ESCC . | Treatment for ESCC and other metastases . | Prognosis . | Author . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 50, M | TC, DC | Detection of a tumor mass | Left hemicolectomy | Metachronous (1Y2M after the first OP) | Lt, Mt | Mod | SE. 8M after SE, CRT for cervical LN metastasis | 5M died | Maruyama et al. [1] |
| 2 | 56, M | DC | Ileus | Left hemicolectomy | Metachronous (9M after the first OP) | Lt | Wel | SE followed by FP and 50 Gy | 9M died | Totsuka et al. (1998) (PJM) |
| 3 | 56, M | TC | Intraoperative detection | Partial resection of the colon | Synchronous | LtAe | Mod | SE followed by FP | 2M died | Shinohara et al. (2000) (PJM) |
| 4 | 70, F | TC-DC | Ileus | Left hemicolectomy | Metachronous (2Y2M after the first OP) | Mt | Mod | SE followed by 45 Gy | Unknown | Horikawa et al. (2001) (PJM) |
| 5 | 74, M | S | Ileus | Hartmann OP | Metachronous (2Y11M after the first OP) | Ae | Mod | SE. 2Y11M after SE, liver metastasis | Unknown | Mizutani et al. (2008) (PJM) |
| 6 | 73, M | S | Ileus | Hartmann OP | Metachronous (1Y after the first OP) | Lt | Por | SE. 11M after SE, CRT for metastasis to the gastric tube | 14M died | Ogaki et al. (2008) (PJM) |
| 7 | 59, F | Ce | Dermatomyositis | Ileocecal resection | Metachronous (1Y after the first OP) | Mt | SCC | SE followed by FP | Unknown | Yamamoto et al. (2009) (PJM) |
| 8 | 60, M | TC | Intraoperative detection | Segmental resection of the colon | Synchronous | Mt | Mod | CRT for ESCC. Local excision of gastric metastasis | Unknown | Karwasra et al. [2] |
| 9 | 51, M | S | Bloody stools | Chemotherapy | Synchronous | MtLtAe | Mod | CRT | 1Y alive | Iwase et al. [3] |
| 10 | 64, M | TC-DC | Asymptomatic | Partial resection of the colon | Synchronous | Mt | Por | CRT and SE | 2.5M died | Our case |
AC, ascending colon; TC, transverse colon; DC, descending colon; Ce, cecum; S, sigmoid colon; Ut, upper thoracic esophagus; Mt, middle thoracic esophagus; Lt, lower thoracic esophagus; Ae, abdominal esophagus; Wel, well-differentiated squamous cell carcinoma; Mod, moderately differentiated squamous cell carcinoma; Por, poorly differentiated squamous cell carcinoma; SCC, squamous cell carcinoma; LN, lymph node; SE, subtotal esophagectomy; FP, fluorouracil and cisplatin; OP, operation; CRT, chemoradiation; PJM, Proceedings of Japanese Meetings.
Four patients with synchronous metastasis of esophageal cancer to the colon have been reported previously, and our patient is the first case that was asymptomatic and diagnosed preoperatively. Of the remaining three patients, two patients were diagnosed intra-operatively and one patient was diagnosed by bloody stools. The prognosis of resection patients including our patient was very short. Only one CRT patient survived for more than a year. Because the number of patients with this type of metastasis described previously is small, there is no operative indication for synchronous metastasis. Even if colonic metastasis is considered to be well controlled and the postoperative course is uneventful, operative stress for esophagectomy may induce an immunosuppressive state.
Of the six metachronous patients described, four patients were diagnosed with colonic obstruction, one with a palpable tumor mass and one with dermatomyositis. Regarding metastasis, five patients had multiple lesions, one had multiple colonic metastases in the transverse colon and descending colon, two had gastric wall metastasis or gastric tube metastasis and only one had liver metastasis. No patients had lung or bone metastasis. Although the prognosis of metachronous cases was also short, one patient survived for more than a year. Thus, operative indication for metachronous colonic metastasis may exist in certain cases. Detecting circulating tumor cells or evaluating the anti-tumor immune response may help in predicting the prognosis of these patients.
Histological differentiation was not observed with ESCC. Furthermore, no specific features were noted in the location of ESCC or site of colonic metastasis. Therefore, there is no clinical marker that predicts colonic metastasis.
In conclusion, our findings suggest that even with well-controlled and asymptomatic colonic metastasis from primary esophageal lesions, the prognosis of patients with primary ESCC is poor. More cases are needed to evaluate the operative indication of such patients.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
ACKNOWLEDGEMENTS
We thank Dr Shiori Demura for checking the data at our local hospital. We also thank Mr David A. Coolidge for English editing.



