-
PDF
- Split View
-
Views
-
Cite
Cite
Christy E. Cauley, Philip J. Spencer, Pallavi Sagar, Allan M. Goldstein, Giant mesenteric lymphatic malformation presenting as small bowel volvulus, Journal of Surgical Case Reports, Volume 2013, Issue 9, September 2013, rjt083, https://doi.org/10.1093/jscr/rjt083
Close - Share Icon Share
Abstract
Abdominal pain with bilious emesis is an ominous clinical presentation with many possible causes. We describe a previously healthy 4-year-old boy who presented with these symptoms and ultrasound findings of fluid throughout most of the abdominal cavity. Computed tomography imaging revealed a large cystic mass (21-by-13 cm) associated with a small bowel obstruction due to volvulus. A laparoscopic exploration was undertaken, revealing a large mass arising from the small intestinal mesentery and causing a segmental volvulus of the small bowel. Conversion to mini-laparotomy allowed reduction of the volvulus and segmental resection of the small bowel associated with a giant mesenteric lymphatic malformation. This case describes a rare cause of intestinal volvulus due to a mesenteric lymphatic malformation.
INTRODUCTION
Lymphatic malformations are benign lymphatic duct masses lined with endothelium and supported by smooth muscle fibers [1]. The majority of childhood lymphatic malformations are located in the neck (75%) and axilla (20%), with the remaining 5% arising from the peritoneal cavity, retroperitoneum and mediastinum [2]. The most common location for an abdominal lymphatic malformation is the small bowel mesentery, with the omentum being second [3]. Mesenteric lymphatic malformations are responsible for 1:20 000 to 1:250 000 hospital admissions. Most patients present within the first 2 years of life with episodic abdominal pain, intermittent vomiting, or increased abdominal girth [4]. Rare cases of intestinal obstruction, volvulus and acute pancreatitis from larger lesions have been described [5–7].
CASE REPORT
A 4-year-old previously healthy male presented to an outside hospital with 2 days of nausea and bilious emesis. An abdominal plain film (Fig. 1a) revealed small bowel obstruction and an abdominal ultrasound was nondiagnostic. Upon transfer to our institution, he had persistent bilious emesis with periumbilical abdominal pain. His medical and surgical history was unremarkable, with no history of antecedent trauma. His mother noted an increasing abdominal girth over the prior several months, but did not seek medical attention. On physical examination, the child's abdomen was soft, mildly distended and with periumbilical tenderness. He had no rebound tenderness or guarding, and no hernias were present. Review of the ultrasound revealed extensive intra-abdominal fluid. An abdominal computed tomography (CT) scan was obtained and revealed a large intraperitoneal cystic mass measuring 13 × 21 × 9 cm in the left abdomen (Fig. 1b). A small bowel obstruction was also present with concern for volvulus due to mesenteric swirl seen on axial imaging. There was no evidence of compromised intestine on CT (Fig. 1c). The patient was taken to the operating room for laparoscopy. The cyst, which arose from the mesentery of the small intestine, resulted in a segmental volvulus with congestion of the involved segment (Fig. 2a–c). A short vertical midline incision was made to allow the giant cyst to be delivered and the volvulus reduced. After reduction, the congested small bowel returned to a normal appearance. The cyst was excised by removing the 8 cm segment of small bowel from whose mesentery it arose (Fig. 2c). The abdomen was closed and the patient was discharged in excellent condition.
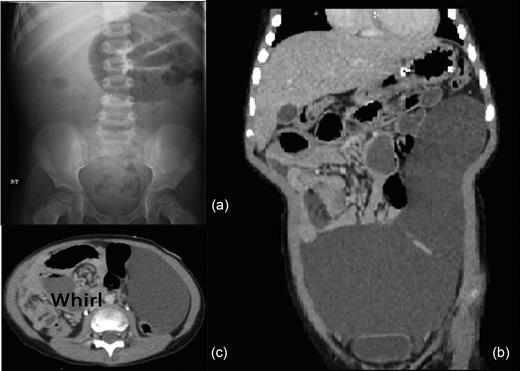
(a) Abdominal X-ray revealing small bowel obstruction in the left upper quadrant. (b) Abdominal-pelvic CT coronal image revealing 13 × 21 × 9 cm intraperitoneal cystic lesion. (c) Abdominal-pelvic CT axial image shows the classic whirl of mesenteric volvulus.
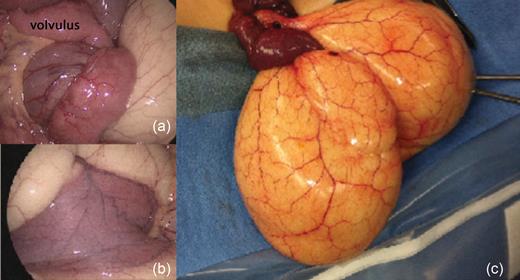
(a) Laparoscopic image of small bowel volvulus at base of lymphatic malformation. (b) Segment of small intestine with lymphatic malformation arising from its mesentery. (c) Intraoperative image of lymphatic malformation after partial aspiration of chylous fluid to allow delivery through the incision.
Pathologic inspection of the mass revealed a thin-walled cyst containing milky fluid. Immunohistochemistry showed that the cyst lining expressed D2–40 (a marker of lymphatic endothelium), but was negative for keratin, WT-1 and calretinin, confirming the diagnosis of lymphatic malformation (Fig. 3).

Histologic cross-section of the surgical specimen after staining for D2–40 expression confirming the lymphatic origin of the cystic lesion.
The patient continues to do well with no postoperative complications at 7-month follow-up.
DISCUSSION
Cystic lymphatic malformations of the small bowel mesentery are uncommon intra-abdominal lesions in children with an unknown incidence. Mesenteric lymphatic malformations account for <1% of all lymphatic malformations [4]. These masses have a variable presentation ranging from asymptomatic to intermittent abdominal pain, vomiting, or peritonitis. Large lesions, as in our case, can cause obstructive symptoms due either to mass effect or, rarely, to volvulus [8].
The diagnosis of lymphatic malformation can usually be made by ultrasonography. These lesions appear as cystic multiloculated masses with thin septae. Rarely, they can have solid components or calcifications likely secondary to internal hemorrhage or infection [9]. Ultrasound is the preferred first-line imaging modality due to its low cost and avoidance of radiation, especially in the pediatric population. In our case, ultrasound diagnosis was limited due to the size of the cyst. Cross-sectional imaging with CT or magnetic resonance imaging (MRI) is useful for further characterization and differentiation from other types of intra-abdominal masses. CT was helpful in this case, identifying a large intraperitoneal cyst with bowel obstruction and a mesenteric swirl consistent with volvulus, thereby prompting emergent operation.
The treatment of lymphatic malformations varies depending on the location of the mass and its symptomatology. Complete surgical excision is the treatment of choice for symptomatic lesions in the abdomen to minimize the risk of recurrence and may require excision of the adjacent bowel [10]. In some cases, complete excision is not feasible due to proximity to vital structures, especially for lesions in the neck. Sclerotherapy is an alternative option in those instances [8].



