-
PDF
- Split View
-
Views
-
Cite
Cite
Venkatesh Subramanian, Pandelis Athanasias, Shreelata Datta, Aziz Anjum, Carolyn Croucher, Surgical options for the retrieval of a migrated intrauterine contraceptive device, Journal of Surgical Case Reports, Volume 2013, Issue 9, September 2013, rjt072, https://doi.org/10.1093/jscr/rjt072
Close - Share Icon Share
Abstract
The intrauterine contraceptive device is a popular form of contraception for women; however, it does carry a rare but serious risk of migration into the myometrium and then into the peritoneal cavity. We report an unusual case of an intrauterine contraceptive device (IUCD) migrating through the uterus into the peritoneal cavity and subsequently into the sigmoid colon, which was finally retrieved laparoscopically. We also discuss three different methods for the retrieval of a migrated IUCD: colonoscopy, hysteroscopy and laparoscopy and compare and contrast each method.
INTRODUCTION
The intrauterine contraceptive device is one of the most widely chosen contraceptive option with over 99% effectiveness in preventing pregnancy, low side effect profile and low cost. However, it is associated with a serious risk of migration into the myometrium of the uterus and potentially into the intraperitoneal cavity and surrounding viscera. This is associated with risk factors including postpartum uterus, retroverted uterus and uteruses with small or irregular endometrial cavities as well as operator's experience. Rarely, an intrauterine contraceptive device (IUCD) may further migrate into the small or large bowel. There are other case reports of an IUCD migrating into the sigmoid colon [1].
Removal of an IUCD that has migrated into or past the myometrium should be strongly considered even in asymptomatic patients because of the dangers of migrating coil as well as risks from adhesion formation such as bowel obstruction and infertility [2, 3].
CASE REPORT
A 27-year-old woman with a previous history of two uneventful vaginal deliveries opted for an IUCD (copper coil) as form of contraception. The coil was fitted easily by an experienced family planning physician. During a routine check 6 weeks later the threads of the coil were not visible on speculum examination. An abdominal X-ray confirmed the presence of the coil in the pelvis. To further specify its location, transvaginal ultrasound scan was performed, which showed an IUCD perforating through the uterine serosa. The patient reported no abdominal pain or irregular vaginal bleeding. After a consultation with the gynaecologist she agreed to proceed for the retrieval of the coil by either hysteroscopy or laparoscopy.
During the hysteroscopy 4 weeks later there was no evidence of an IUCD into the uterine cavity and no evidence of a perforation site in the uterus (Fig. 1). A laparoscopy followed, locating the coil threads deep in the Pouch of Douglas, with the IUCD perforating through the sigmoid colon into the lumen (Fig. 2). The IUCD was retrieved laparoscopically and the defect in the sigmoid colon was repaired by stapling the tear (Fig. 3).

Hysteroscopy showing a normal endometrial cavity, no evidence of IUCD or site of perforation.
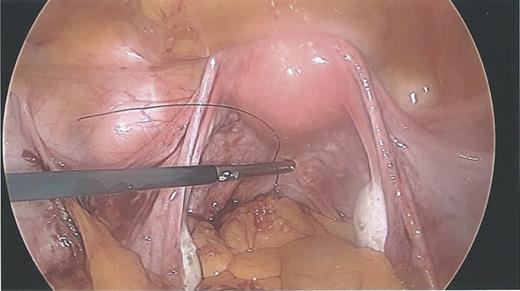
Laparoscopy showing normal IUCD threads deep inside the Pouch of Douglas inside the sigmoid colon.
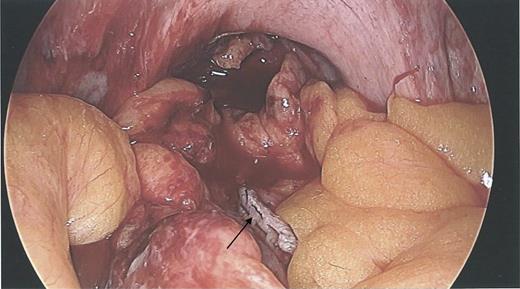
Laparoscopy showing a sigmoid colon post-repair after removal of coil.
The patient made a non-eventful postoperative recovery and was discharged after 72 h of observation.
DISCUSSION
There are many ways to retrieve an IUCD depending on the location of the device and on the potential involvement of the peritoneal cavity structures. We discuss three methods for the retrieval of a migrated IUCD: hysteroscopy, laparoscopy and colonoscopy.
Hysteroscopy
When an IUCD has migrated through the myometrium of the uterus it is possible to remove the device during a hysteroscopy, even when it appears deeply embedded. It has also been reported that an IUCD embedded in a submucous myoma can be resected with a hysteroscope, removing the myoma together with the IUCD. However, if an IUCD has perforated through the uterine serosa and breaches into the peritoneal cavity, a laparoscopic approach is necessary to minimize the risk of trauma to surrounding tissues and deal with potential bleeding [4, 5].
Laparoscopy
Laparoscopy remains the gold standard for management of an IUCD that has perforated through the uterus. Assistance from general surgeons or urologists may be necessary when there is involvement of the bowel or the urinary tract. Occasionally endoscopic management may not be suitable when there are significant adhesions or due to the anatomical location of the IUCD and an exploratory laparotomy is warranted. However, a laparoscopic approach facilitates a quicker post-operative recovery as demonstrated in this case. In either case it is important to observe the patient closely postoperatively for any signs of bleeding or peritonitis, secondary to repair of any damaged organ [6].
Colonoscopy
When an IUCD has migrated into the rectum or colon, removal of the IUCD with a colonoscope or sigmoidoscope has been reported. Retrieval of an IUCD by this method has not resulted in spillage of bowel contents, peritonitis or fistula formation according to the literature. This has been thought to be due to a combination of omental adhesions formation, as well as an inflammatory response [7].
We have discussed three different methods for the retrieval of an IUCD that has migrated outside the uterine cavity. Table 1 summarizes the advantages and disadvantage of each method. An IUCD in the peritoneal cavity carries the risk of causing bowel obstruction, adhesions formation, damage to intra-abdominal organs, infection, fistula and bleeding. Laparoscopy and hysteroscopy remain the mainstay of management of IUCD's that have migrated into and past the uterine myometrium. However, colonoscopy does provide a novel management option for IUCDs that have migrated into the large bowel lumen, with potentially reduced surgical morbidity.
| . | Advantages . | Disadvantages . |
|---|---|---|
| Hysteroscopy | Can be done as outpatient | Unable to visualize or remove if IUCD migrated past serosa or embedded in peritoneal structures |
| Can be done without sedation or regional anaesthesia | ||
| Laparoscopy | Clear anatomical identification of IUCD if in the peritoneal cavity | More invasive than hysteroscopy and colonoscopy |
| Ability to potentially repair damaged intra-abdominal organs | Unable to visualize IUCD if in the lumen of bowel or bladder | |
| Colonoscopy | Less invasive than laparoscopy | Only possible when IUCD in the lumen of bowel |
| Potentially reduces surgical morbidity | Need to convert to laparoscopy or laparotomy | |
| Can be done under sedation |
| . | Advantages . | Disadvantages . |
|---|---|---|
| Hysteroscopy | Can be done as outpatient | Unable to visualize or remove if IUCD migrated past serosa or embedded in peritoneal structures |
| Can be done without sedation or regional anaesthesia | ||
| Laparoscopy | Clear anatomical identification of IUCD if in the peritoneal cavity | More invasive than hysteroscopy and colonoscopy |
| Ability to potentially repair damaged intra-abdominal organs | Unable to visualize IUCD if in the lumen of bowel or bladder | |
| Colonoscopy | Less invasive than laparoscopy | Only possible when IUCD in the lumen of bowel |
| Potentially reduces surgical morbidity | Need to convert to laparoscopy or laparotomy | |
| Can be done under sedation |
| . | Advantages . | Disadvantages . |
|---|---|---|
| Hysteroscopy | Can be done as outpatient | Unable to visualize or remove if IUCD migrated past serosa or embedded in peritoneal structures |
| Can be done without sedation or regional anaesthesia | ||
| Laparoscopy | Clear anatomical identification of IUCD if in the peritoneal cavity | More invasive than hysteroscopy and colonoscopy |
| Ability to potentially repair damaged intra-abdominal organs | Unable to visualize IUCD if in the lumen of bowel or bladder | |
| Colonoscopy | Less invasive than laparoscopy | Only possible when IUCD in the lumen of bowel |
| Potentially reduces surgical morbidity | Need to convert to laparoscopy or laparotomy | |
| Can be done under sedation |
| . | Advantages . | Disadvantages . |
|---|---|---|
| Hysteroscopy | Can be done as outpatient | Unable to visualize or remove if IUCD migrated past serosa or embedded in peritoneal structures |
| Can be done without sedation or regional anaesthesia | ||
| Laparoscopy | Clear anatomical identification of IUCD if in the peritoneal cavity | More invasive than hysteroscopy and colonoscopy |
| Ability to potentially repair damaged intra-abdominal organs | Unable to visualize IUCD if in the lumen of bowel or bladder | |
| Colonoscopy | Less invasive than laparoscopy | Only possible when IUCD in the lumen of bowel |
| Potentially reduces surgical morbidity | Need to convert to laparoscopy or laparotomy | |
| Can be done under sedation |



