-
PDF
- Split View
-
Views
-
Cite
Cite
Kristin L. Long, Carol Spears, Daniel E. Kenady, Branchial cleft cyst encircling the hypoglossal nerve, Journal of Surgical Case Reports, Volume 2013, Issue 9, September 2013, rjt068, https://doi.org/10.1093/jscr/rjt068
Close - Share Icon Share
Abstract
Branchial cleft anomalies are a common cause of lateral neck masses and may present with infection, cyst enlargement or fistulas. They may affect any of the nearby neck structures, causing compressive symptoms or vessel thrombosis. We present a case of a branchial cleft cyst in a 10-year-old boy who had been present for 1year. At the time of operation, the cyst was found to completely envelop the hypoglossal nerve. While reports of hypoglossal nerve palsies due to external compression from cysts are known, we believe this to be the first report of direct nerve involvement by a branchial cleft cyst.
INTRODUCTION
Branchial cleft cysts are congenital lesions often presenting as lateral neck masses. Up to 95% of branchial cleft anomalies originate from the second branchial cleft [1]. Cysts that originate from the second or third cleft are in anatomic intimacy with vital neck structures such as the carotid artery, jugular vein and hypoglossal nerve [2, 3]. Despite this, involvement of neighboring structures and concomitant complications are exceedingly rare. Surgical excision is the definitive treatment for branchial anomalies and is often performed without complication [4]. Isolated case reports of internal jugular vein thrombosis and hypoglossal nerve palsies secondary to compression have been reported [5, 6]. We present a case of a branchial cleft cyst completely encircling the hypoglossal nerve.
CASE REPORT
A 10-year-old African boy presented with complaints of left-sided anterior neck swelling for 1year. The swelling was non-tender, not associated with any prior trauma and had no drainage or sinus tract. The patient reported occasional shortness of breath and a history of snoring, but was otherwise in good health. He had no prior medical or surgical history, no allergies and took no medications. He was the fifth born in a family of seven children. On physical examination, the patient was alert and in no distress. He had a prominent non-tender swelling in the left anterior neck, measuring 8 cm by 5 cm. The remainder of his physical examination was unremarkable, as were vital signs and basic laboratory values.
After obtaining informed consent from the parents, the patient was taken to the operating room with a diagnosis of a branchial cleft cyst. After incision, a large cystic mass was easily identified. During dissection of the cyst, it was noted that a structure appeared to pass through the cyst (Fig. 1A). This was identified as the hypoglossal nerve. The cyst was found to completely encircle the hypoglossal nerve. With careful dissection and eventual transection of the cyst anterior to the nerve, the cyst was removed and the hypoglossal nerve remained intact (Fig. 1B). Rupture of the cyst was necessary to release the nerve at the time of excision. The completion of the procedure was uneventful and the patient recovered from general anesthetic without incident. On postoperative day 1, he was noted to have mild left-sided tongue deviation, suggesting hypoglossal nerve palsy. No hypoglossal nerve palsy was present preoperatively. He remained otherwise asymptomatic and was discharged home in stable condition.
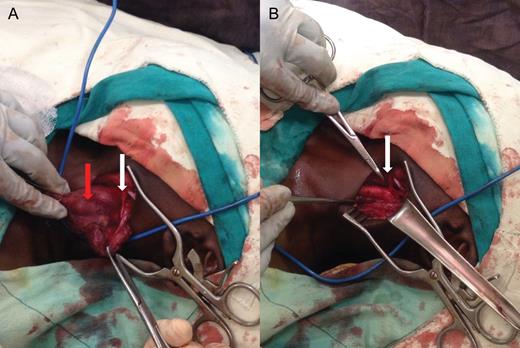
Intraoperative images of left neck (cranial to caudal from right to left). (A) The branchial cleft cyst in situ (red arrow), with the hypoglossal nerve indicated by the white arrow. (B) The left neck after removal of the cyst, with the intact nerve visible at the tip of the hemostat (white arrow).
DISCUSSION
Branchial cleft anomalies arise from deviations in the complex embryologic development of the anterior and lateral neck regions. The development of the second arch takes place over a more extended time period and anomalies in this region are more common [3]. A thorough understanding of the embryology and origin of the branchial clefts explains the proximity of cysts, sinuses and fistulae to the vital structures of the neck. Cysts, in particular, often present as rapidly enlarging neck masses, and may be prone to repeated infections if not excised early. The inflammatory response produced in such infections has been proposed as one mechanism for the few reports of hypoglossal nerve involvement by branchial cleft cysts [6]. Extremely large cysts can also extrinsically compress nearby structures, causing nerve palsies and vessel thrombosis.
Careful dissection in the neck is of paramount importance, and the identification of all structures encountered during cyst excision must be carried out. Meticulous dissection allowed us to recognize an unexpected structure involved with the branchial cleft cyst and subsequently preserve the nerve. In our case, the patient had no prior symptoms indicating a nerve involvement, and the intraoperative finding was unexpected. This case serves to remind surgeons that direct involvement of any of the surrounding neck structures should be anticipated and prepared for branchial cleft excisions.



