-
PDF
- Split View
-
Views
-
Cite
Cite
Abdullah Almulaifi, Waleed M. Mohammad, Obstructive jaundice: a rare complication of laparoscopic greater curvature plication, Journal of Surgical Case Reports, Volume 2013, Issue 8, August 2013, rjt062, https://doi.org/10.1093/jscr/rjt062
Close - Share Icon Share
Abstract
Laparoscopic greater curvature plication (LGCP) is relatively a new procedure. We report a novel complication of obstructive jaundice in a 24-year-old patient post LGCP. This was secondary to gastric mucosa prolapse with obstruction of the ampulla of Vater. A literature review revealed no previous reports of similar complication.
INTRODUCTION
Morbid obesity is a major health problem worldwide [1]. Bariatric surgery is currently the most effective mean of excess weight loss. Surgical procedures are associated with complications. We report obstructive jaundice as a complication of LGCP.
CASE REPORT
A 24-year-old female, who had undergone laparoscopic greater curvature plication (LGCP) 6 months earlier, presented to the emergency room with 1 day history of severe epigastric pain, associated with nausea. She also complained of yellow discoloration of skin and dark urine.
On examination, she was jaundiced. Vital signs were as follows: temperature 38°C, heart rate 120 bpm, blood pressure 140/87. Abdominal examination revealed marked tenderness at the epigastric and peri-umbilical areas, with guarding. White blood cells count was 12.8 × 109/l and haemoglobin count was 109 g/l. Renal profile was within normal. Total bilirubin was elevated at 74.1 mmol/l, and the reminder of liver function test was within normal.
An ultrasound of abdomen showed distended gallbladder with no calculi, dilated CBD and mild intra-hepatic biliary radicles dilatation. Stomach and duodenum were shown to be grossly dilated. The CT scan of the abdomen showed gastric outlet obstruction with an abnormal position of gastro-duodenal junction. Gastric mucosal prolapsed with mass effect on duodenum (and ampulla of Vater) and secondary dilatation of the biliary and pancreatic ducts.
Upper GI endoscopy showed the status post gastric plication with herniation of gastric fold into the duodenum. An attempt was made to manipulate the fold but was not successful (Fig. 1).

The patient underwent exploratory laparotomy, and anterior gastrotomy. The mucosal fold was delivered relieving the obstruction. The redundant mucosa was transacted by a linear cutter stapler (Fig. 2) and the gastrotomy closed primarily.
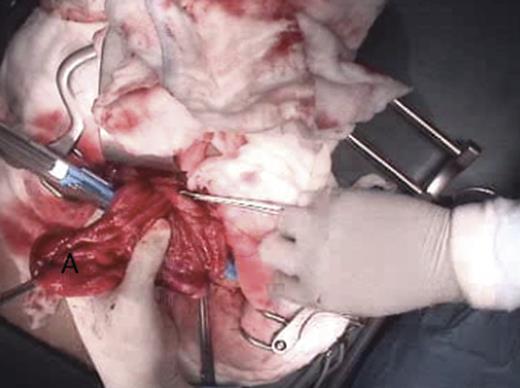
Intra-operative picture of the obstructing gastric mucosal fold (A) being prepared for transection.
The post-operative course was unremarkable, with gradual normalization of total bilirubin.
DISCUSSION
Many types of restrictive operative procedures have been performed to achieve weight loss [2]. Newer operations and techniques are being developed. LGCP is relatively a new technique. It was first proposed in 1981 by Wilkinson [3] and popularized by Talebpour [4]. The procedure remains investigational [5]. Two major variations of this technique have been reported [6]. The anterior plication (AP) involves the plication of the anterior wall of the stomach without the mobilization of the greater curvature and the greater curvature plication (GCP) in which the short gastric vessels are divided and the greater curvature is folded inward. The GCP appears to be superior in weight loss comparing with AP [6].
Our patient had undergone LGCP. The greater omentum was taken off the greater curvature of the stomach starting just proximal to the pylorus using an energy device. The short gastric vessels were also divided. A 38 French calibration tube was passed by the anaesthetist from the mouth traversing the pylorus. Using about 4–5 interrupted 2-0 absorbable sutures, the greater curvature was folded. A second running continuous suture was then applied. The calibration tube insured maintaining a fixed diameter lumen at the entire length of the stomach. At the end of the procedure, methylene blue dye test was performed to rule out any leak associated with suturing.
LGCP attempts to mimic the well-documented results of laparoscopic sleeve gastrectomy. In our case, the weight loss was about 19 kg over 6 months. LGCP has the potential advantages of absence of staple line and its risk of leak. The operation also forgoes the use of costly endoscopic staplers. Many series have been reported in literature with varying number of patients [7].
Different procedure-related complications have been reported. These include perforation, obstruction, permanent nausea and vomiting, intracapsular abscess, sialoreia, GI bleeding and partial jejunal necrosis [8, 9].
Different series have described gastric outlet obstruction as a complication secondary to fold herniation [8]. No precipitating factors were identified in our patient. There were no specific complaints in four follow-up visits prior to presentation to the emergency room. To our knowledge, we report the first case of obstructive jaundice as a long-term complication of LGCP. The mechanical obstruction of the ampulla of Vater was secondary to fold herniation. An endoscopic attempt of reduction may be of value as previously reported in the literature [10]. It was not successful in our case. However, once the herniation was corrected surgically, the jaundice gradually resolved.
In conclusion, different complications associated with LGCP are still being reported. The procedure remains investigational and should be performed under the research ethic review board approval.



