-
PDF
- Split View
-
Views
-
Cite
Cite
Kristin L. Long, Cortney Y. Lee, Chand Ramaiah, David A. Sloan, Intrapericardial parathyroid adenoma, Journal of Surgical Case Reports, Volume 2013, Issue 8, August 2013, rjt064, https://doi.org/10.1093/jscr/rjt064
Close - Share Icon Share
Abstract
Primary hyperparathyroidism from a parathyroid adenoma is common. Ectopic parathyroid glands have been reported in numerous locations, including the chest. We present a single case report of an intrapericardial parathyroid gland found after failed bilateral neck exploration. The patient presented with severe, recurrent nephrolithiasis and acute renal failure prior to his surgical intervention. Repeat imaging identified a parathyroid adenoma in the mediastinum that was localized to the aortopulmonary window. After attempts at minimally invasive thoracotomy and posterolateral thoracotomy, a median sternotomy was ultimately required to identify the adenoma.
INTRODUCTION
Primary hyperparathyroidism is the most common cause of hypercalcemia in the ambulatory setting, occurring in both men and women most commonly in the sixth decade. Prevalence is now estimated at 1 in 500 women and 1 in 2000 men [1]. Approximately 85% of primary hyperparathyroidism cases are caused by a solitary parathyroid hormone-secreting adenoma. Adenomas are found in ectopic locations in 16% of cases [2]. Common locations of ectopic parathyroid adenomas range from the tracheo-esophageal groove, thymus, thyroid, to the mediastinum [2]. Symptomatology in hyperparathyroidism includes fatigue, weakness, abdominal pain, depression and commonly nephrolithiasis [3]. The presence of kidney stones, especially when recurrent, is considered an indication for operative intervention in primary hyperparathyroidism [4]. We present a case of an ectopic parathyroid adenoma in the pericardium causing complicated nephrolithiasis and acute renal failure.
CASE REPORT
A 32-year-old male was referred to the endocrine surgery team with hypercalcemia and a history of several years of kidney stones. He had first been diagnosed with elevated serum calcium ∼6months prior to his visit in the endocrine surgery clinic but had experienced recurrent problems with nephrolithiasis for several years prior to this. He underwent three lithotripsy procedures and multiple urologic stent placements during this time. Additional symptoms included severe fatigue, weakness and joint pain. Aside from his nephrolithiasis and subsequent renal failure, the patient was otherwise healthy, with no medication use, no allergies, and no history of tobacco or alcohol use.
Six months prior to our evaluation, at another hospital, the patient underwent failed neck exploration for primary hyperparathyroidism. Pre-operative imaging suggested a right inferior parathyroid adenoma, but bilateral neck exploration including a right thyroid lobectomy was unsuccessful. The initial operation was complicated by transient bilateral vocal cord palsies. The patient was evaluated by an otolaryngologist, and his weak voice and vocal cord palsies resolved without any further intervention.
His hypercalcemia persisted and the patient continued to suffer from nephrolithiasis. Despite his multiple urologic interventions, he developed renal failure with a creatinine peaking at 13.5 and requiring temporary dialysis. Parathyroid imaging, including sestamibi/SPECT scan as well as MRI/MRA of the neck and chest suggested an ectopic parathyroid adenoma in the aortopulmonary window (Fig. 1). Following consultation with cardiothoracic surgery, the patient underwent a minimally invasive thoracic approach to the mediastinum, followed by conversion to a left posterolateral thoracotomy. Neither approach located the suspected mediastinal adenoma. A median sternotomy was then performed. The entire thymus and all mediastinal fatty tissues were removed without evidence of any abnormality. Finally, the pericardium was opened and a 0.610 g starfish-shaped parathyroid adenoma removed without complication (Figs 2 and 3). The patient's intraoperative PTH levels dropped precipitously from 400 to 53 pg/ml. The patient recovered uneventfully and was discharged home on calcium supplementation. At 6-month follow-up, no further evidence of renal stone disease was noted on imaging.
Sestamibi/SPECT imaging indicating a parathyroid adenoma in the mediastinum
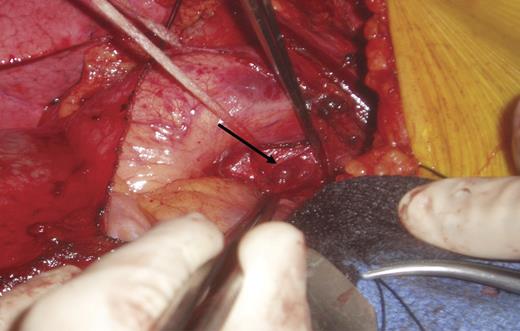
Intraoperative photograph showing the cut edge of the pericardium and the parathyroid adenoma just lateral to the aortic root (arrow)

DISCUSSION
Although mediastinal parathyroid glands are common, to our knowledge, only one other case of an intrapericardial adenoma has been reported [5]. Inferior parathyroid glands are more frequently found in ectopic locations, ranging from the superior mediastinum to the aortopulmonary window to the carina. The inferior glands, which develop from the third pharyngeal pouch and normally migrate caudally with the thymus, may also remain undescended and have been found as high as the angle of the mandible. The higher incidence of ectopic inferior parathyroid glands is often attributed to this abnormal migration during embryogenesis [6]. Reports indicate that 1–2% of ectopic parathyroid glands have been found within the mediastinum and may be treated with video-assisted thoracoscopic surgery, open thoracotomy or median sternotomy, if necessary [7]. Adenomas are occasionally found within the aortopulmonary window, which places them lateral to the ductus arteriosus and extrapericardial in location. These are often felt to represent supernumerary parathyroid glands and one embryologic theory ties their development to migration with the recurrent laryngeal nerve [8]. Increasing use of radionuclide imaging has proved beneficial in identifying parathyroid adenomas in ectopic locations. Likewise, advent of selective venous sampling procedures, intraoperative gamma probe use and 4D computed tomography scans have all increased the likelihood of accurate localization, especially after failed neck exploration. An intrapericardial parathyroid gland, while highly unusual, serves to highlight the tremendous variety of possible ectopic locations. This unique case reinforces the challenges associated with persistent primary hyperparathyroidism after failed neck exploration.
Conflict of interest statement. No conflicts of interest exist for the authors of this manuscript.
REFERENCES
Author notes
Case presented as ‘Romancing the Stones’, American Association of Endocrine Surgeons Annual Meeting, 14 April 2013, Chicago, IL, USA.



