-
PDF
- Split View
-
Views
-
Cite
Cite
Gerusa O.M. Cardoso, Edgard Matta-Neto, Vivian N. R. El Achkar, Walter Niccoli-Filho, Aggressive osseous commitment result by keratocyst odontogenic tumour: case report, radiographic and clinical standpoints, Journal of Surgical Case Reports, Volume 2013, Issue 7, July 2013, rjt044, https://doi.org/10.1093/jscr/rjt044
Close - Share Icon Share
Abstract
Keratocystic odontogenic tumour (KCOT) previously known as odontogenic keratocyst was recently classified as a benign lesion characterized by an infiltrating pattern, local aggressiveness with the propensity to recurrence. It is thought to arise from the dental lamina. Pain is usually not associated with KCOT until swelling occurs, and it commonly affects the posterior mandible. Multiple KCOT are associated with nevoid basal cell carcinoma syndrome. This study reports an aggressive case of KCOT with destruction of the osseous tissue of the mandible, accentuated face asymmetry, dysphagia and dysphonia. It was managed with a defined protocol which entailed diagnosis, treatment with enucleation along with peripheral ostectomy and rehabilitation. A long-term follow-up schedule was provided to the patient to observe the recurrence behaviour of this cyst. In postoperative phase, no complication was noticed regarding wound healing and recurrence.
INTRODUCTION
Both solitary cases and syndrome-related cases are recently named keratocystic odontogenic tumour (KCOT) (WHO Classification of Head and Neck Tumours, 2005). KCOT is a rare and benign but locally aggressive developmental cystic neoplasm [1]. It most often affects the posterior mandible and is generally thought to be derived from either the epithelial remnants of the tooth germ or the basal cell layer of the surface epithelium [2]. Swelling is the most common presenting complaint; however, KCOTs may be asymptomatic and found incidentally on dental X-rays.
The differential diagnoses consist in odontogenic cyst, dentigerous cyst and ameloblastoma (radiologically). Malignant transformation to squamous cell carcinoma may occur, but is unusual [2, 3].
The opinions about how to treat KCOTs differ. Among then excisional biopsy, marsupialization, curettage and Carnoy's solution were mentioned and the follow-up of the patient is mandatory [1, 2].
This case reports an aggressive case of KCOT with destruction of the osseous tissue of the mandible, accentuated face asymmetry, dysphagia and dysphonia.
CASE REPORT
A 40-year-old male Caucasian patient coming to the Department of Biosciences and Diagnosis of Sao Paulo State University–UNESP to evaluate an increase of volume in a left side of the face and neck with pain, dysphonia and dysphagia symptoms. The extra oral clinical exam showed an extensive oedema in region of mandible, relatively hard to palpation, with no committal of the skin and no lymphadenopathy. The intra oral examination showed a large mass in the vestibular region that extended to the middle of the mandible until the ascendant ramous, tender to palpation, oedema and mobility of the present teeth. A punch with a needle in a hypodermic syringe showed a viscous liquid with yellowish colour and high internal pressure. Immediately after the decompression, the skin diminished considerably.
Three-dimensional images allowed for the visualization of the lesion in relation to relevant anatomical structures providing depiction of bone destruction in the body of the mandible. Preoperative 3D CT reconstruction indicated destruction of the buccal cortex of the mandible (left side) caused by the lesion and projection of osseous spiculae (Fig. 1A and B).
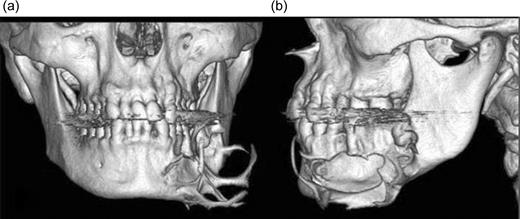
Frontal view of pre-operatory 3D CT images shows the destruction of bone and a spiculars osseous formation (a) and in lateral view show the destruction of the cortex (b).
The panoramic radiography shows a large radiolucent and well-defined lesion with a radiopaque corticates margin involving the left mandibular premolar and molar (Fig. 2).
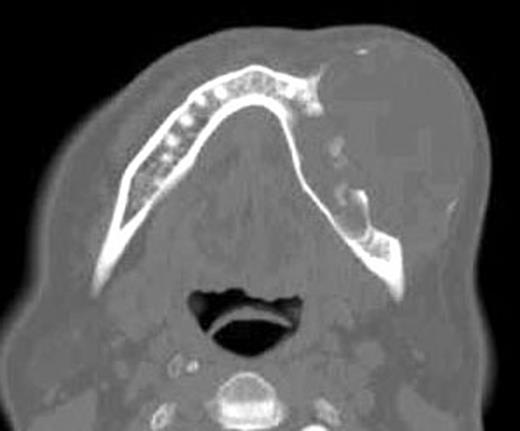
Preoperative axial CT view shows the lesion with destruction the medullar and buccal cortical portions of the left mandible.
The clinical, radiolological and tomography signs (Fig. 3) evoke the hypothesis of a KCOT or ameloblastoma. An incisional biopsy and cytological smears were done and the results showed thin epithelial layer, composed of from 8 to 10 cell. The basal layer shows palisade organized cells with a uniform nucleus. In the direction of the cyst lumen, there is parakeratosis with a focal zone created of orthokeratins. The palisading appearance of the basal cells was evident and confirms the diagnosis of KCOT.

The panoramic radiography shows a large radiolucent and well-defined lesion with a radiopaque corticates margin involving the left mandibular premolar and molar area.
The patient was sent to a Maxillofacial Surgery Department and after the clinical and laboratorial routine examinations, a vigorous curettage washed with Carnoy solution as well as an ostectomy and removal of all the osseous spiculae before the marsupialization was done. A resin obturator was made and was fixed in the mucosa by suture in order to not allow the closure of the mucosa and to permit the patient to clean the lumen with 9% NaCl solution in a hypodermic syringe through the marsupialization aperture and return each 3 months to follow up and makes new radiographic examinations. After 6 months, the radiographic examinations show an initial osseous organization and the clinical appearance have no signal of infection or recurrence.
DISCUSSION
Maxillary and mandibular cysts are very common due to the presence of odontogenic epithelium remnants [1, 2, 4]. The main difference among KCOT and other cysts is their potentially aggressive behaviour, recur more often than any other type of jaw cyst [5, 6] and are almost comparable with that of the ameloblastoma [5, 6]. The average recurrence rate is 30% [5], and a recurrence rate as high as 62% has been reported [5–7].
The presence of residual epithelium or an epithelial remnant after the treatment is one of the suspected contributing factors for the high recurrence rate or a presence of satellite cysts in the cyst's wall. Zachriades et al. [7] conclude that the KCOT do not develop through an increase in osmotic pressure in the lumen like other cysts and Brannon [8] affirmed that they have an active epithelial lining with a more rapid rate of proliferation than that of radicular cysts.
Elevated level of oxidative enzymes and acid phosphatase increased cell activity which indicates high metabolic and lysosomal activities. In addition, the KCOT connective tissue walls have an increased level of the collagenase enzyme leucine aminopeptidase [5].
The treatment of the KCOT is another challenge because despite being a benign tumor, the potential of recurrence is high and can come to transform in a malignant tumour. Bataineh and al Qudah [6] advocate jaw resection as the favourable treatment. Different treatments have been recommended, ranging from enucleation to resection without a continuity defect [6]. The marsupialization and enucleation to en bloc resection is used with success. According to Schmidt and Pogrel [9] and Ortakoúlu [10], the ideal treatment for the odontogenic keratocyst would be enucleation or curettage followed by treatment of the cavity with an agent such as liquid nitrogen or Carnoy solution to eliminated the epithelial remnants or satellite cysts.
The potential for recurrence of the KCOT relates to the high proliferate activity of the keratocyst epithelium. Due to the high recurrence rate and aggressive behaviour of KCOT, different treatment techniques can be chosen.
A postoperative follow-up with regular radiographic examination is mandatory because of the potential for recurrence. This lesion usually recurs within 5 years after surgery, but they can recur >15 years later.
In this case of KCOT, we had success by means of aggressive curettage and marsupialization. There was no sign of recurrence on follow-up for 1 year. The patient has been symptom free up to now and he is under long-term review.



