-
PDF
- Split View
-
Views
-
Cite
Cite
Monique A. Gary, Jacqueline Wu, Marcella Bradway, The space between: a supralevator abscess caused by perforated diverticulitis, Journal of Surgical Case Reports, Volume 2013, Issue 6, June 2013, rjt041, https://doi.org/10.1093/jscr/rjt041
Close - Share Icon Share
Abstract
Supralevator abscesses are the rarest manifestation of anorectal suppurative disease. We report a supralevator abscess in a 60-year-old male whose earliest presentation included poorly localized abdominal and pelvic pain, tenesmus, urinary retention and weight loss, initially treated as diverticular disease based upon imaging and presentation. Progressive symptoms led to the discovery of a pelvic abscess with subsequent percutaneous drainage, later followed by emergent laparotomy, where a single perforated diverticulum was revealed to be the source fistulization. He underwent a Hartmann procedure with concomitant drainage of supralevator and ischiorectal collections. Perirectal pain with neurological involvement is part of a constellation of signs and symptoms that should invoke a high index of clinical suspicion for supralevator abscess formation. Percutaneous attempts at drainage are often inadequate; definitive surgical therapy is the best approach to prevent recurrence and associated morbidity.
INTRODUCTION
Suppurative disease of the anorectum is common. Out of the documented regions in which this disease is known to exist (perianal, intersphincteric, ischiorectal, submucosal and supralevator) [1] supralevator abscesses account for only 3–4% of total disease incidence [2, 3]. Risk factors for the development of abscesses in this location include male gender, obesity, diabetes, immunodeficiency, malignancy, foreign bodies, tuberculosis, trauma and inflammatory bowel disease [3–6]. Although few, they are most severe in their clinical course and consequence, with perianal sepsis often necessitating surgical intervention due to inadequate initial drainage [2]. We report the unique presentation of a supralevator abscess with extension into the ischiorectal fossa secondary to perforated diverticulitis, with emergent surgery required after unsuccessful percutaneous drainage.
CASE REPORT
A 60-year-old male presented to our institution with a 4–6-week history of progressive constipation, painful defecation, urinary retention and increasing lower abdominal pain and pressure. He described some associated nausea, chills and tenesmus after small, frequent movements. Additionally, this patient relayed ∼8-lb weight loss over a 2-month period secondary to decreased oral intake and fear of painful and incomplete evacuation, and had begun experiencing pelvic and sacral pain when sitting. His past medical history included hypothyroidism, anxiety, hypercholesterolemia and smoking. On physical exam the patient demonstrated tenderness to palpation across the lower abdomen without evidence of peritonitis. Digital rectal examination revealed an enlarged prostate, good sphincter tone; significant tenderness upon palpation of the rectum was elicited, with no purulent drainage expressed.
Contrast-enhanced computed tomography (CT) scan revealed the presence of diverticulosis and perirectal mesenteric stranding concerning for diverticulitis (Fig. 1); therefore, the patient was admitted and treated empirically for the same with i.v. antibiotics. He was discharged several days later with a 2-week course of amoxicillin clavulanate.
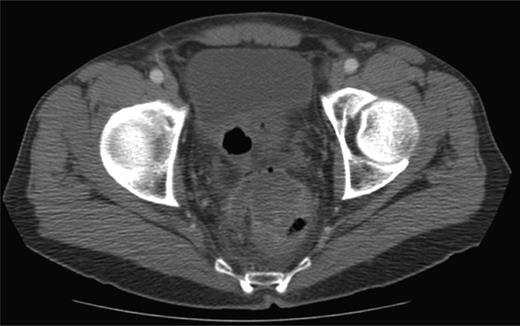
CT scan depicting perirectal stranding without definite abscess formation.
In the 6-week follow-up, repeat CT demonstrated eccentric thickening of the rectosigmoid with interval development of an adjacent complex pelvic fluid collection with supralevator extension measuring 3.5 × 2.5 cm (Fig. 2a and b). Percutaneous needle biopsy revealed pus, and a drainage catheter was left in place (Fig. 3a and b). The patient did not improve, was reimaged and was found to have collection extending into the ischiorectal fossa and supralevator space (Fig. 4). Owing to refractory pain and persistent leukocytosis, the patient was taken to the operating room for examination under anesthesia. No fistulous tract or internal drainage was noted within the rectal vault; however, consistent with the imaging, external induration was observed along the right ischiorectal fossa, where, upon incision, a large purulent cavity was evacuated. On evening rounds, the patient was noted to have a marked leukocytosis and frank stool coming from the ischial wound, and he was taken emergently to the operating room for diagnostic laparotomy where a perforated diverticulum adherent to the pelvic sidewall was identified (Fig. 5). Therefore, a Hartmann procedure, drainage of supralevator abscess, irrigation and debridement of the right ischiorectal wound, was performed.
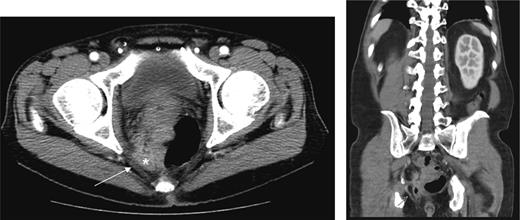
(a) Repeat CT at 6 weeks showing supralevator abscess formation (white asterisk). The levator ani muscle is illustrated by white arrow (b) coronal image of complex supralevator collection. Arrow points to the levator ani muscle.
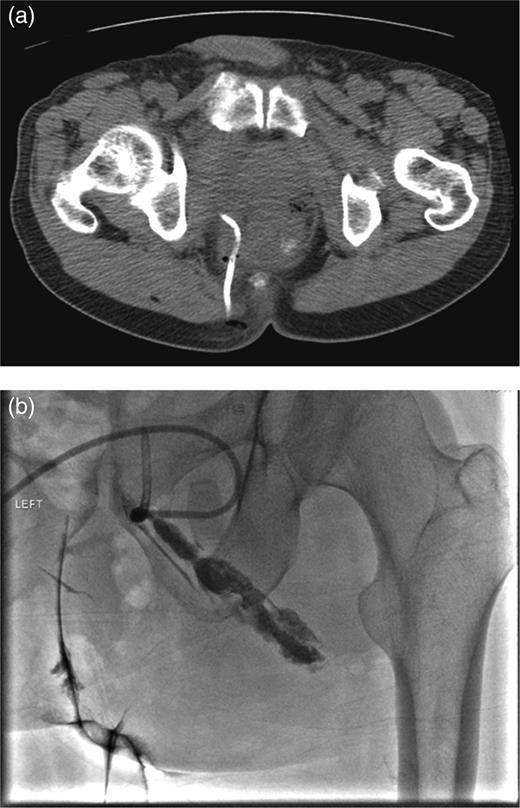
(a) CT-guided percutaneous drainage of perirectal abscess (b) fluoroscopic drain study showing contrast extending into the supralevator space.
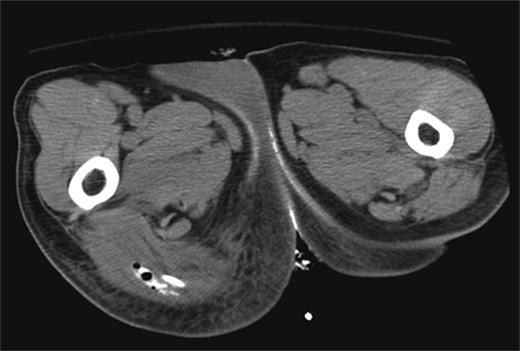
CT scan demonstrating ischiorectal extension of oral contrast and air tracking.

Intraoperative specimen. Sigmoid colon, etc colon with single perforated diverticulum separated from the right pelvic sidewall at the site of fistulization.
DISCUSSION
Work up of any suspected anorectal abscess begins with a thorough history and physical exam. Data from previous case reports and retrospective analyses highlight a common constellation of signs and symptoms that are quite common in most cases of pelvic suppuration including pain (gluteal, perianal), fever, leukocytosis and drainage. These, however, invoke little clinical suspicion of supralevator involvement, though the additive complaint of neurological impairment (urinary retention, deep pelvic/sacral and/or sciatic pain) may be important clues to aid in diagnosis [7]. Imaging modalities, including CT or MRI, should be utilized to make the correct diagnosis, with drainage as the primary treatment.
Drainage of a supralevator collection poses more challenge than other types of anorectal abscesses [2]. These collections lie within a closed potential space between the pelvic floor (peritoneal reflection) and the levator ani muscles, lateral to the walls of the rectum [8], making adequate drainage via a transrectal approach difficult, with high recurrence rates. Concomitant ischiorectal drainage may result in a complex fistula that can be difficult to manage [2]. Although percutaneous, trans-sciatic drainage of a supralevator collection could result in outward spread along the lateral fascial planes of the ischiorectum (as in this case), the anatomical boundaries of this closed space make the reverse scenario unlikely; a primary ischiorectal collection would be drained superficial to the supralevator space, never entering it, while deep to the supralevator space lies the lateral wall of the rectum itself, making internal catheter drainage especially challenging. The absence of either internal or external communication underscores the perils associated with incomplete drainage. Inadequate initial management may lead to sepsis; therefore, an open transabdominal approach, albeit more invasive, can ensure visualization of the anatomy necessary to provide definitive treatment of supralevator infection [9]. A thorough knowledge of anorectal anatomy and heightened index of suspicion in the face of a somewhat subtle presentation can prevent delay in diagnosis and may result in reduced morbidity for patients with this complex disease.
REFERENCES
- weight reduction
- abscess
- diverticulum
- laparotomy
- pain
- pelvic pain
- suppuration
- surgical procedures, operative
- urinary retention
- abdomen
- diagnostic imaging
- morbidity
- pelvic abscess
- diverticulosis
- hartmann operation, rectal resection
- abscess, supralevator
- tenesmus
- perforated diverticulitis
- diversion procedure



