-
PDF
- Split View
-
Views
-
Cite
Cite
Harsh A. Kanhere, Markus I. Trochsler, John Pierides, Guy J. Maddern, Atypical mycobacterial infection mimicking metastatic cholangiocarcinoma, Journal of Surgical Case Reports, Volume 2013, Issue 6, June 2013, rjt038, https://doi.org/10.1093/jscr/rjt038
Close - Share Icon Share
Abstract
Mycobacterial infections are rare in developed countries. Isolated involvement of the liver and biliary tree by mycobacterial infection is extremely rare. We report a case of a 45-year-old Caucasian female presenting with obstructive jaundice with a common bile duct stricture and multiple hypodense liver lesions raising suspicion of a metastatic cholangiocarcinoma. Percutaneous core biopsies of the liver lesions however suggested granulomatous process and histology at surgical excision confirmed this finding. Atypical mycobacteria (M. abcessus) sensitive to Amikacin were cultured from the surgical specimen proving the diagnosis. With the resurgence of tubercular and atypical mycobacterial infections in the developed world, it is important not to overlook these in differential diagnosis of various malignancies.
INTRODUCTION
Mycobacterial infections are rarely seen in developed countries [1]. Whilst some cases of tubercular granulomas of the liver [2, 3] have been reported, isolated involvement of the biliary tree and liver by atypical mycobacteria is extremely rare.
Almost all reports are from developing countries [4]. Atypical mycobacteria causing localized liver and biliary tree involvement and mimicking metastatic cholangiocarcinoma has never been reported according to our knowledge.
This entity is very rarely considered as a differential diagnosis for biliary strictures and liver lesions in the western world and consequently a very high index of suspicion is necessary to make a diagnosis.
CASE REPORT
A previously fit and healthy 45-year-old Caucasian female presented to our unit with history of jaundice, mild upper abdominal discomfort and weight loss. She had undergone a laparoscopic cholecystectomy 5 years ago followed by an endoscopic retrograde cholangiopancreatography (ERCP) to extract a common bile duct (CBD) calculus. There was no history of overseas travel or contact with patients with tuberculosis.
The liver function tests revealed an obstructive picture. Bilirubin level was 86 µmol/l (normal 2–24 µmol/l). Gamma glutamyl transferase (GGT) and alkaline phosphatase were 347 and 340 U/l, respectively. In view of prior history of choledocolithiasis, an ERCP was undertaken. An eccentric stricture at the level of the junction of cystic duct and CBD was seen along with a dilatation of proximal the bile duct. There were no ductal calculi. A plastic stent was inserted to relieve the jaundice (Fig. 1). These findings raised the suspicion of a malignant process, and a computerized tomography (CT) scan of the chest, abdomen and pelvis was consequently performed.

The CT scan revealed multiple hypodense liver lesions predominantly in the right lobe of the liver (Segment 6 and 8) highly suspicious of metastatic deposits (Fig. 2). A preliminary diagnosis of metastatic cholangiocarcinoma was made on this basis.
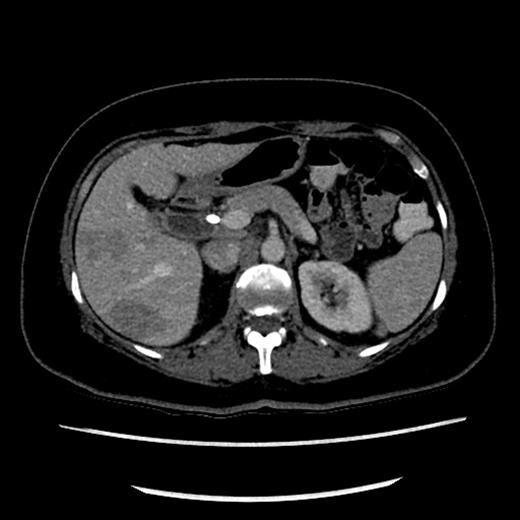
CT scan showing hypodense lesions in the liver with CBD stent in situ.
The case was discussed in the multidisciplinary meeting and decision was taken to attempt a percutaneous biopsy of the liver lesions to confirm the diagnosis and plan for palliative chemotherapy.
An ultrasound-guided core biopsy was attempted, but failed due to technical reasons. A CT-guided core biopsy of Segment 6 lesion was successful, but an interval reduction in the size of the liver lesions was noted. A magnetic resonance cholangiopancreatography (MRCP) to reassess the liver and biliary tree was therefore planned. MRCP revealed a persistent stricture at the cystic duct CBD junction (Fig. 3). The histology from the core biopsies of the liver revealed a granulomatous process with Langhans giant cells (Fig. 4). The pathologists opined that although rare, mycobacterial involvement should be considered as a differential diagnosis. This coupled with the spontaneous reduction in the size of the liver lesions led to a consensus opinion for a surgical exploration to resect the biliary stricture and re-biopsy the liver lesions.

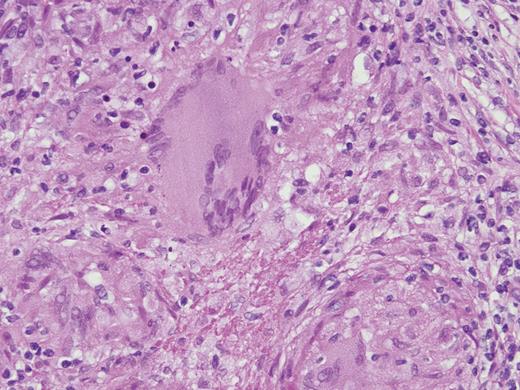
Core biopsy of the liver showing granuloma with Langhans giant cells.
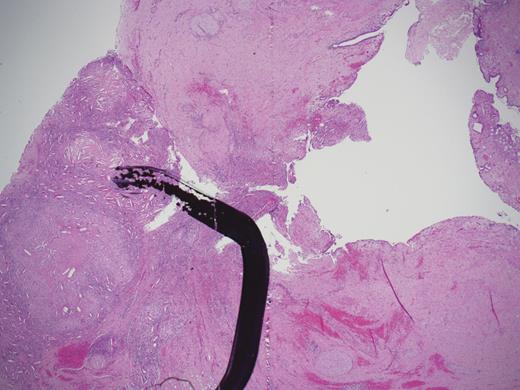
At surgery multiple liver lesions were evident and two of these were biopsied. A fibrotic stricture was evident in the mid-portion of the CBD with proximal dilatation.
Surgical resection of the stricture was undertaken with a Roux-en-Y hepaticojejunostomy. Since the possibility of Mycobacterial granulomas had been raised, a sample of tissue from the resected specimen was sent for mycobacterial culture.
Liver biopsies confirmed granulomatous inflammation. Histology of the resected biliary stricture showed granulomas causing wall thickening and structuring of the bile duct. The mucosa was uninvolved (Fig. 5). No malignancy was evident. Tissue sent for culture grew Mycobacterium abcessus sensitive only to Amikacin. There was no suggestion of immunodeficiency and HIV testing was negative. The patient was commenced on therapy and is currently progressing very well.
DISCUSSION
Tuberculosis and atypical mycobacterial infections are a re-emerging problem in both developing and developed countries [5]. An estimated one-third of the world population is infected and 2 million people die of the disease each year [5].
In Australia, the incidence of tuberculosis is low [1] (4.1–4.9 per 100 000 population per year). The exact incidence of atypical mycobacterial infections is unknown, but non-tubercular mycobacteria are more prevalent in the western world than tuberculosis [6]. Mycobacterium abcessus is the most pathogenic and chemotherapy resistant rapid growing mycobacterium [7].
In immunocompetent hosts typically after trauma M. abcessus predominantly causes soft tissue infections [8]. Another pattern is that of chronic respiratory disease with fibrosis. Systemic immunosuppression can predispose to disseminated disease [8].
This case is an unusual presentation of M. abcessus infection affecting the hepatobiliary system in isolation in an immunocompetent patient. Mycobacterium abcessus is ubiquitously found in the environment and commonest method of infection is through trauma. Minor trauma causing inoculation followed by haematogenous spread to the hepatobiliary system is a possible hypothesis for this presentation.
This case underlines the need for appropriate diagnostic workup for all liver lesions. The accuracy of diagnosing liver lesions radiologically approaches 95% depending on the modality used [9]. While contrast-enhanced CT and MRI coupled with PET scan are sufficient in diagnosing metastatic disease in most instances, a core biopsy to confirm histology is mandatory when the diagnosis is in doubt. The present case is an excellent example of importance of histological confirmation of the diagnosis of a liver lesion.
There is an increasing need to include mycobacterial infections in the differential diagnosis in developed countries with evolving epidemiology and drug resistance of such infections.
REFERENCES
- amikacin
- nontuberculous mycobacteria
- cancer
- cholangiocarcinoma
- biliary tract
- common bile duct
- constriction, pathologic
- developed countries
- differential diagnosis
- mycobacterium infections
- mycobacterium infections, atypical
- european continental ancestry group
- diagnosis
- histology
- liver
- jaundice, obstructive
- core needle biopsy
- excision
- hepatic lesions
- surgical specimen



