-
PDF
- Split View
-
Views
-
Cite
Cite
Kentaro Shimodaira, Yasuyuki Miyakura, Ai Sadatomo, Chieko Miyazaki, Hideki Sasanuma, Koji Koinuma, Hisanaga Horie, Yasuo Hozumi, Alan T. Lefor, Yoshikazu Yasuda, Penetration of a divided cystoperitoneal shunt catheter into the transverse colon inducing acute mastitis, Journal of Surgical Case Reports, Volume 2013, Issue 5, May 2013, rjt039, https://doi.org/10.1093/jscr/rjt039
Close - Share Icon Share
Abstract
We report a rare case of acute mastitis caused by enteric organisms passing through a cystoperitoneal shunt catheter, which had penetrated into the colon. The patient is a 56-year-old woman who underwent shunt placement for cyst formation after surgery for meningioma at the age of 29. After 26 years, she suffered from a brain abscess and an attempt was made to surgically remove the indwelling catheter. Only part of the catheter could be removed, leaving a divided and ligated catheter in situ. A year later, she described right-breast pain. CT showed that the catheter had migrated into the colon, followed by colonoscopy confirming that the catheter had indeed penetrated the colon. The breast to the abdomen segment of the catheter was exteriorized through the right-anterior chest wall without laparotomy. A patient who presents with acute mastitis and has previously undergone shunt surgery should have a careful assessment of the entire catheter.
INTRODUCTION
Ventriculoperitoneal and cystoperitoneal (CP) shunts are commonly used for the treatment of hydrocephalus and symptomatic intracranial cysts. These procedures are associated with various complications including ventriculitis, meningitis and abdominal complications. Abdominal complications, including intestinal volvulus, pseudocyst formation and migration into the gastrointestinal tract have been reported, accounting for 25% of shunt-related complications. Bowel perforation by the shunt catheter is uncommon and accounts for 0.01–0.07% of all abdominal complications [1–3]. Breast-related complications represent a class of thoracic shunt complication and are characterized by breast cerebrospinal fluid (CSF) pseudocyst formation, CSF galactorrhoea and shunt obstruction [4]. We report a rare case of acute mastitis caused by enteric organisms passing through a CP shunt catheter, which had penetrated the transverse colon, and was related to a previous failed attempt to remove the shunt resulting in a divided catheter.
CASE REPORT
The patient is a 56-year-old woman who underwent a surgical treatment of a lateral ventricle meningioma at the age of 29. A month later, she underwent CP shunt placement for cyst formation after resection. The postoperative course was uneventful and she was well without shunt-related problems for 26 years. She developed a brain abscess related to the shunt catheter at the age of 55. A surgical removal of the catheter was attempted, but was not technically possible, and only the segment from the clavicle to the breast was removed with ligation of the two remaining ends. The two disconnected catheter segments remained in situ and were not retrieved. A year later, she was taken to a local hospital with continuous right-breast pain. The diagnosis of acute mastitis was made and she was referred to our institution for further examination. On presentation, her right breast was swollen with erythema (Fig. 1). There was no abdominal pain and change in bowel habits. Funduscopic evaluation was normal with no signs of increased intracranial pressure. Her temperature was 36.7°C, and laboratory tests revealed a decreased platelet count of 103 000/μl, elevated AST of 97 U/l, ALT of 72 U/l and C-reactive protein level of 1.4 mg/dl. The breast abscess was drained under local anesthesia. Cultures taken from the abscess showed enteric organisms including Enterococcus avium, Klebsiella oxytoca and Bacillus. Abdominal CT showed that the shunt catheter was in the splenic flexure of the transverse colon with no other abnormalities (Fig. 2). Colonoscopy was performed to survey the colon and the shunt catheter was found inside the lumen at the splenic flexure (Fig. 3). Acute mastitis caused by enteric organisms which had migrated through the shunt catheter after penetration into the transverse colon was the presumptive diagnosis, and the catheter removed under general anesthesia. The breast to the abdomen segment of the catheter was exteriorized through the right-anterior chest wall without laparotomy. The postoperative course was uneventful. She was transferred to local hospital 15 days later.

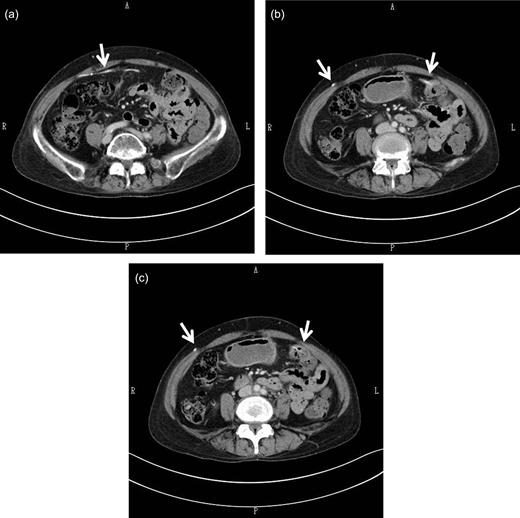
Abdominal CT scan findings. The shunt catheter (white arrow) extended through the right-rectus sheath (a), crossed the midline to the left side of the abdomen (a, b) and was inside the splenic flexure of the colon (b, c). There was no free air or other abnormalities in the abdominal cavity.
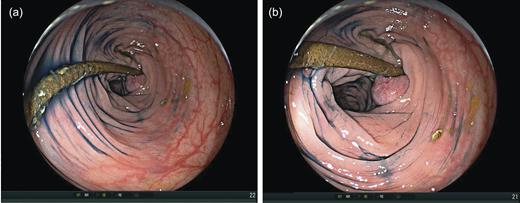
Colonoscopy showed the distal catheter within the transverse colon, ∼40 cm proximal to the anal verge (a). An inflammatory polyp was present at the penetration site in the colon wall (b).
DISCUSSION
The penetration of shunt catheters into the intestine at the distal end is rare with a reported incidence between 0.01 and 0.07% [1]. The mortality rate may be high, up to 15%, due to intracranial or intra-abdominal infections. It can occur within a few weeks to several years after shunt surgery. Several factors have been found to be responsible for this rare complication, including chronic irritation of the gastrointestinal tract, prior abdominal surgery or silicone allergy [2, 3]. Breast-related complications involving the thoracic segment of catheter are also rare [4]. CSF leakage and retrograde flow from the peritoneal cavity to the breast may cause breast-related complications. This is the first report of case with acute mastitis caused by enteric organisms migrating through a CP shunt catheter that had penetrated the transverse colon.
The diagnosis of bowel perforation by a shunt may not be easy to make, unless the shunt protrudes from the anus [5, 6]. Prolonged diarrhea of unknown etiology, as well as abdominal symptoms, serves as warning signs of possible bowel perforation. CT can play a crucial role in the diagnosis of bowel perforation. In the present case, the diagnosis of penetration into the transverse colon was confirmed by CT. The cultures taken from the right-breast abscess revealed enteric organisms. These findings suggested that the infection was due to the retrograde flow from the colon. Colonoscopy showed a penetrating tube inside the lumen of the colon. The development of mastitis was facilitated by previous division of the catheter, leaving a ligated end. Presumably, the ligature became dislodged, leaving a direct connection from the breast tissue to the distal end of the catheter.
Several methods to treat bowel perforation due to shunt migration have been reported [6]. The choice of treatment depends on the clinical presentation. In the present case, the shunt catheter was directly removed percutaneously. The removal of the shunt may allow the spontaneous closure of the bowel defect. Previous study reports that the shunt catheter can be directly removed percutaneously in 69% (31/45), whereas 17% (8/45) of patients require a laparotomy and repair of the bowel [1]. If there is evidence of significant abdominal infection, such as an abscess or life-threatening peritonitis, the fistulous opening may not close spontaneously, warranting laparotomy.
In the present case, previous insufficient surgical treatment such as a partial removal of the catheter contributed to this shunt-related complication. However, it is common surgical practice to permit the distal end of a shunt catheter to remain in situ in order to simplify the surgical procedure. These catheters typically remain as free-floating tubes within the peritoneal cavity. Although this practice is most commonly uncomplicated, it is not unreasonable to suspect that the tube may irritate the serosal surface of the colon leading to chronic inflammation. It is speculated that local inflammation owing to repeated irritation of the bowel wall by the catheter tip might have contributed to the subsequent perforation.
In conclusion, a patient who presents with acute mastitis and has previously undergone shunt placement should undergo assessment of the abdominal segment of the catheter.



