-
PDF
- Split View
-
Views
-
Cite
Cite
Robert Tyler, Ross Vint, Lawrie Morton, Beware: the inguinoscrotal hernia with urological origins, Journal of Surgical Case Reports, Volume 2013, Issue 2, February 2013, rjt001, https://doi.org/10.1093/jscr/rjt001
Close - Share Icon Share
Abstract
Cases of herniated bladder diverticulae causing inguinoscrotal hernias are rare, and there are 19 described in the English literature. We describe the case of a 64-year-old Caucasian man with a huge bladder diverticulum that herniated into his scrotum. The original diagnosis was that of inguinoscrotal hernia containing bowel contents. Radiological investigations revealed a urological cause, and he underwent a successful diverticulectomy. It is important to recognize that inguinoscrotal hernias can have urological origins, 1–4% being the reported figure. Clinical examination can lead to a general surgical diagnosis before further radiological investigations confirm the nature of the hernia. They prove difficult to both diagnose and surgically correct.
INTRODUCTION
Inguinoscrotal hernias containing bladder diverticulae are rarely seen. From searching Pubmed and Medline, we found 19 other published cases. We report the case of a 64-year-old gentleman with lower urinary tract symptoms and a left-sided herniated bladder diverticulum causing an inguinoscrotal hernia. He underwent a diverticulectomy, which was performed successfully, and was discharged 5 days post-operatively. His follow-up ultrasound confirmed bladder emptying to completion with no further diverticulae or herniation of any kind.
CASE REPORT
Our patient was a 64-year-old gentleman who complained of nocturia, diurnal frequency, poor flow and terminal dribbling. This was associated with and intermittent left scrotal swelling. He had a medical history of late-onset asthma, erectile dysfunction and hypertension.
When seen at clinic, he was found to have a left scrotal swelling that extended into the inguinal region associated with a cough impulse. It was felt that this was either a hydrocele or a sliding hernia and an USS was arranged. His uroflometry showed that he had an obstructed flow, but he emptied his bladder on post-residual scanning. In addition to the USS, he was commenced on an alpha-blocker for bladder outflow obstruction and a flexible cystoscopy was arranged.
His USS diagnosed an inguinal hernia containing omental fat. At this point a referral to a general surgeon was made. His cystoscopy showed a normal urethra with a small, short prostate and a high bladder neck. The bladder itself was unusual. Upon filling a large left-sided bladder, diverticulum was seen.
Based on this cystoscopic finding, a micturating cytogram was arranged to evaluate this diverticulum as seen in the figures provided (Figures 1 and 2). This showed an unusual huge bladder diverticulum that had herniated through his inguinal canal, filling his left hemiscrotum.
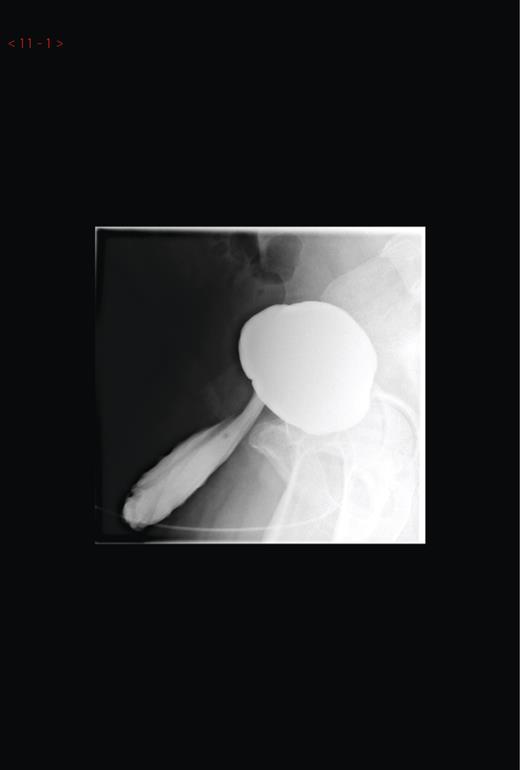
Micturating cystourethrogram showing contrast in the left hemiscrotum.

Micturating cystourethrogram showing contrast in the left hemiscrotum.
This was obviously contributing to his urinary symptoms by having a reservoir that could not be emptied on micturition. It was felt that this could deteriorate, and surgical excision was agreed with the patient.
Surgery
Our aim was to perform a diverticulectomy with repair of the hernia defect. For this we used a retropubic lower midline incision. Dissection was made down onto the bladder until the diverticulum was identified. Dissection was attempted to remove the diverticulum off the outer bladder surface and spermatic cord as it entered the deep inguinal ring. Unfortunately, the diverticulum was adherent to adjacent structures and this was not possible.
To confidently identify the neck of the diverticulum, the bladder was therefore opened and held with stay sutures. This allowed dissection of the adhesions between the outer surface of the bladder and the diverticulum. However, it was not possible to identify the spermatic cord at this stage; therefore, the neck of the diverticulum was transected in order that a point of traction was created.
This facilitated dissection with a combination of blunt and sharp technique. The spermatic cord was identified and safely separated from the hernial sac including the diverticulum. The plane was followed into the scrotum where the entire diverticulum was removed from the hemiscrotum. There were no adhesions within the scrotum of the diverticulum to surrounding layers, which made a secondary scrotal incision unnecessary. Haemostasis was ensured in these areas and the bladder was closed with two layers of continuous vicryl.
Two weeks following the procedure he underwent a trial of voiding, which he passed successfully. He was discharged home and returned 6 months later with for a follow-up ultrasound of his renal tract, which revealed no further pathology.
DISCUSSION
A case review of inguinal hernias with urological causes was carried out in 2003, finding 190 cases, with only 10 documenting bladder diverticulae. Of the remaining 180 cases, 116 contained bladder, while 64 contained ureter [1]. We have found nine more since this.
Inguinal hernias are a common finding in a general surgical clinic, with a lifetime risk of 27% in men and 3% in women [2]. Of these, 1–4% have urological origins, increasing to 10% over the age of 50 [3]. Therefore, any patient presenting with an inguinal hernia and lower urinary tract symptoms must have bladder herniation considered. However, many patients with bowel herniation will have concomitant prostatic hyperplasia causing urinary symptoms, while patients with bladder herniation, conversely, can have no urinary symptoms. Patients who are male, obese and over 50 and have multiple urinary symptoms are seen as high risk.
In hernia en glissade any extraperitoneal viscus can pull a sheath of peritoneum with it into the inguinal canal. Ours contained no peritoneum or detrusor muscle and therefore is classed as a pure herniated diverticulum.
On herniating through into the inguinal canal, bladder diverticulae can exacerbate underlying lower urinary tract symptoms and confuse the diagnosis of an inguinal hernia. It must be stressed that these hernias are very unlikely to strangulate due to the presence of a wide neck [4].
On examination of this patient, there was a left-sided scrotal swelling associated with a cough impulse. After clinical examination, current guidelines recommend ultrasound as the first-choice diagnostic test in evaluating testicular and extra-testicular pathology [5].
In addition to an ultrasound, a cystoscopy was arranged as the irritative symptoms continued and this highlighted a huge bladder diverticulum. It has been noted that cystoscopy can overlook bladder diverticulae with narrow necks and miss potential diagnosis [6]. It is recommended that cystography investigates large diverticulae seen on cystoscopy [7].
Inguinoscrotal bladder hernias are generally corrected operatively. Our surgery attempted to perform a diverticulectomy with a repair of the hernia defect. This was complicated by the adhesions between bladder, spermatic cord and diverticulae. It has been reported that the risk of bladder injury is as high as 12% when repairing this type of hernia, these risks comprising haematuria, sepsis, urinary leakage and fistula formation as well as testicular infarction [8]. We experienced no post-operative complications.
In conclusion, this rare case illustrates the complexity of both diagnosing and treating inguinal hernias. It stresses the importance of considering urological causes in high-risk patients and utilizing both ultrasound and cystography to reach a diagnosis. Once diagnosed, these hernias can be successfully repaired but care must be taken intra-operatively to avoid bladder injury.
ACKNOWLEDGEMENTS
I acknowledge the consent of the patient to have his case reported on.
I thank Mr. Ron Alexander, consultant urologist, for the guidance on writing this case report.
Conflict of interest statement. None declared.



