-
PDF
- Split View
-
Views
-
Cite
Cite
Jason Ramsingh, Ahmad Ali, Ahmed Al-Ani, Gerrit Denys, Surgical emphysema following therapeutic colonoscopy, Journal of Surgical Case Reports, Volume 2013, Issue 12, December 2013, rjt118, https://doi.org/10.1093/jscr/rjt118
Close - Share Icon Share
Abstract
Colonoscopy is an invasive procedure used in the detection of colon cancer, inflammatory bowel disease and investigation of bleeding from the rectum. In addition to diagnostic procedures, colonoscopy also has therapeutic indications such as polypectomy and dilation of strictures. We present a case of a patient who presented with cervical emphysema following a therapeutic colonoscopy. The patient had no abdominal or chest pain, shortness of breath and was managed conservatively. Perforation following colonoscopy is a rare complication; however, it is essential that doctors recognize and are aware of the different presentations and management options for this complication.
INTRODUCTION
Colonoscopy is used in the evaluation of diseases affecting the lower gastrointestinal tract. Being an invasive procedure, it is associated with complications that can be managed conservatively or require surgical intervention. In our case report, we discuss a patient who developed surgical emphysema following a therapeutic colonoscopy without any associated abdominal or chest symptoms and was managed conservatively. This case report highlights one of the rare presentations of colonoscopic perforations and provides a feasible management option for clinicians.
CASE REPORT
A 60-year-old female presented to our endoscopy suite after being referred by her general practitioner for investigation of bleeding and passage of mucus per rectum. She also complained of tenesmus and reduced appetite but no weight loss. Her past medical history included being diagnosed with ulcerative colitis 26 years ago during her first pregnancy for which she was treated with steroids and has been relatively healthy since then. She had a previous colonoscopy in 2008, following a positive bowel screening. This colonoscopy showed quiescent colitis confirmed by biopsy. During the present colonoscopy, she had biopsies taken from her rectum, sigmoid, descending and ascending colon given the findings of pseudopolyps.
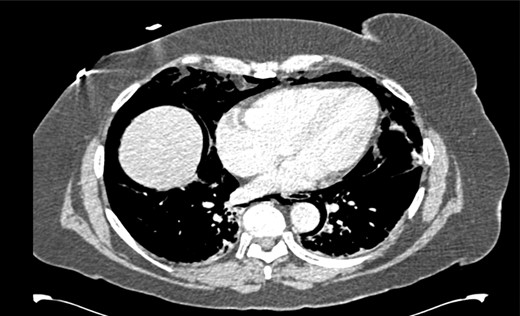
After her procedure she complained of swelling in her neck. This was not accompanied by shortness of breath, chest pain or abdominal pain. On examination, her oxygen saturation was 99% on room air, with normal respiratory and heart rate. Her respiratory examination was normal and her abdomen was soft and non-tender. She had marked crepitus over her clavicles, supraclavicular fossa and most of her neck. Her erect chest X-ray revealed air under both hemidiaphragms and significant pneumomediastinum (Fig. 1). A computed tomography (CT) scan of her chest, abdomen and pelvis was requested. This CT-scan revealed very extensive spreading of surgical emphysema in the retroperitoneum, extending into the mediastinum with small volumes of free intraperitoneal gas (Figs 2–4).
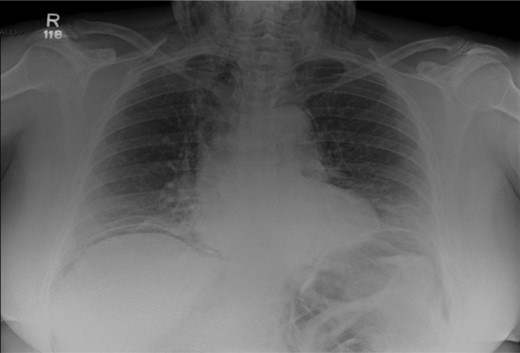
Chest X-ray illustrating pneumoperitonuem, pneumomediastinum and cervical emphysema.


CT scan of abdomen showing free intraperitoneal gas compressing the splenic flexure.
The patient was admitted and managed conservatively. This consisted of keeping her nil by mouth for 24 h, intravenous fluids and antibiotics. Her cervical emphysema gradually resolved and she was discharged 72 h after presentation without any surgical intervention.
DISCUSSION
The rate of perforation following colonoscopy ranges from 0.03 to 0.12% [1, 2]. Perforations can occur from three different mechanisms [3]. First, it can result from mechanical perforation with the colonoscope and is usually recognized at the time of endoscopy. Secondly, it can occur as a result of overzealous air insufflation or barotrauma. Lastly, it can occur after therapeutic procedures such as polypectomies and biopsies.
Various authors have identified significant risk factors for perforation. Arora et al. [4] reported that advanced age, significant comorbidity, obstruction as an indication for colonoscopy and performance of invasive interventions increased the risk of perforation. Rabeneck et al. [5] also reported that older age, male sex, having a polypectomy and a low volume endoscopic service increased the risk of perforation.
Our patient presented after a therapeutic colonoscopy with cervical emphysema as the initial complaint without any abdominal or chest complaints even though her imaging revealed both pneumoperitoneum and pneumomediastinum. Fortunately, she did not exhibit signs of the fourth pneumothorax and did not require a chest drain. This is in stark contrast to previously published case reports where patients developed pneumothoraces requiring chest tube drainage [6, 7].
Maunder et al. [8] has described the path taken by air in the retroperitoneum into the mediastinum. Briefly, air in the retroperitoneum can track upwards entering the mediastinum via the hiatus for the aorta and IVC. The air can then continue along fascial planes into the neck resulting in cervical emphysema. Additionally, air within the peritoneum can enter the mediastinum via the oesophageal hiatus or can pass through openings in the diaphragm to enter the pleural cavity resulting in pneumothorax [9].
Conservative management of perforation following colonoscopy is a safe and acceptable option in patients not exhibiting signs of peritonitis, adequate bowel preparation or silent perforations. Additionally, perforations resulting from therapeutic procedures are usually small and are best managed conservatively [10]. Perforation following colonoscopy is a known but fortunately rare complication. Being aware of the various presentations and management options will improve clinical care.



