-
PDF
- Split View
-
Views
-
Cite
Cite
Hellen McK Edwards, Haytham Al-Tayar, A transmesenteric congenital internal hernia presenting in an adult, Journal of Surgical Case Reports, Volume 2013, Issue 12, December 2013, rjt099, https://doi.org/10.1093/jscr/rjt099
Close - Share Icon Share
Abstract
Congenital internal hernias (CIAHs) are a rare cause of small bowel obstruction in adults. We present a case of transmesenteric CIAH in a 32-year-old male. The clinical examination and computed tomography scan were interpreted as intestinal obstruction, and only an emergency laparotomy revealed that 1 m of small bowel herniated through a 2 cm defect in the mesentery of the transverse colon. Repair of the defect was performed using interrupted suturing, and the patient was discharged after 4 days without sequelae.
INTRODUCTION
The definition of an internal hernia is the protrusion of intestines or other abdominal organs through a mesenteric or peritoneal fossa, occasionally leading to strangulation or incarceration, and is a rare form of both hernia and small bowel obstruction. Autopsy studies report a 0.2–0.9% incidence of internal hernias causing bowel obstruction in 4.1% of all cases [1].These hernias are either congenital or acquired, the latter constituting the majority mainly presenting after liver transplantation or gastric bypass surgery [2, 3]. Congenital internal abdominal hernias (CIAHs) can be classified as either retroperitoneal or formed from congenital anomalous openings, the latter lacking a true peritoneal sac. Retroperitoneal hernias can be subdivided into paraduodenal (30–53% of CIAH), Winslow's foramen (8% of CIAH), paracecal (6% of CIAH) and intersigmoid hernias (5% of CIAH), whereas hernias formed from congenital anomalous openings can be categorized as transmesenteric (5–10% of CIAH), broad ligament (4–7%) or transomental hernias (1–4%). Transmesenteric hernias (TMHs) are the most common internal hernias in children, and are mainly caused by openings in the mesenterium of the small bowel (71% of TMH) and less by mesocolic defects (26% of TMH) [1, 4]. The literature on CIAH is sparse with most cases being reported in children [2, 5], whereas cases in adults are rare [2, 6–10].
Symptoms of intestinal obstruction in CIAH in adults are similar to symptoms due to other causes of intestinal obstruction with acute onset of abdominal pain, nausea, vomiting and tachycardia. We present a case of congenital transmesenteric hernia presenting in an adult.
CASE REPORT
A 32-year-old man undergoing treatment for a depression with serotonin–norepinephrine reuptake inhibitors (SNRIs) and with one prior admission to the hospital due to rightsided abdominal pain was admitted to our department after 4 h with severe abdominal pain. The pain was acute in onset, stabbing and located in the whole right side of the abdomen, radiating to the back and to the right groin. The pain was associated with nausea and restlessness, and could not be reduced with either NSAID or high doses of morphine. On presentation, he was ill looking, sweating, restless and in agony. He was ABC stable, his abdomen distended with generalized tenderness and in his upper right quadrant he had a 10 × 10-cm hard very sore mass, with positive rebound tenderness. There were normal bowel sounds.
Paraclinical tests showed leucocytosis (10,1 × 109/l) and normal serum lactate. A computed tomography (CT) scan showing gastric retention, encapsulated dilated small intestines in the right upper quadrant with pneumatosis intestinalis and collapsed small intestines distally from this area interpreted as intestinal obstruction (Figs 1 and 2).

Coronal view of preoperative abdominal CT scan demonstrating encapsulated dilated small intestines in the right upper quadrant with pneumatosis intestinalis.
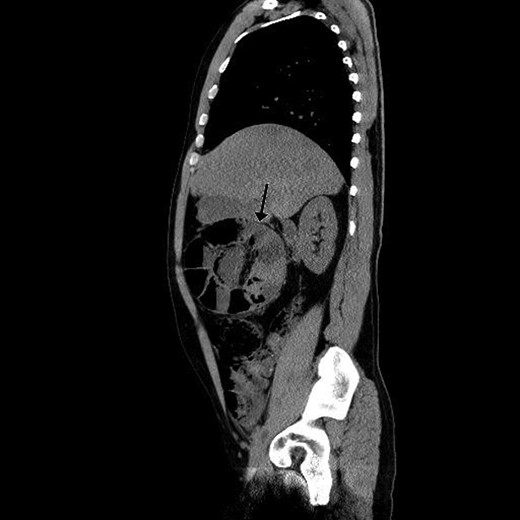
Sagittal view of preoperative abdominal CT scan demonstrating encapsulated dilated small intestines in the right upper quadrant with pneumatosis intestinalis.
An emergency laparotomy was performed 12 h after the first appearance of the symptoms and 7 h after admission to the hospital. This revealed severe small bowel obstruction. Approximately 1 m of small bowel was found distended, herniated and strangulated through a 2-cm defect in the mesentery of the transverse colon. Furthermore, it was capsuled in the mesenteric peritoneum, resembling a balloon ready to burst. The intestines were greyish in colour, but vital without signs of necrosis or ischaemia (Fig. 3). The peritoneal capsule was then removed and the defect widened, before the herniated small bowel could be loosened and retracted back through the hernia. The defect was sutured. The postoperative course was smooth, and the patient was discharged 4 days later. The patient has not been readmitted to the hospital at 18 months follow-up, but did complain of mild pain in the upper abdomen the first few weeks after discharge.

DISCUSSION
The congenital transmesenteric hernia is a rare form of hernia, but has been known for many years, with the first successful operation in 1888 [1]. Our case is identical to the literature, where the defect is described as being circular and 1–3 cm in diameter and presentation is described as severe pain, right-sided abdominal tenderness often revealing a palpable abdominal mass (the Gordian knot of herniated intestine) [1]. Diagnosis is often challenging, due to the nonspecific symptoms. A CT scan may provide suspicion of a transmesenteric hernia, often revealing small bowel dilation, cluster of small bowel loops, central displacement of colon, lack of omental fat overlying the cluster and displacement of the mesenteric trunk. The sensitivity and specificity of diagnosis by CT has been calculated to be ∼63 and 76% [2, 10]. The findings can still be hard to distinguish from other internal hernias, and the diagnosis is therefore often not made until exploration. Surgical repositioning of the strangulated bowel segment as early as possible is the therapy of choice, as delay can lead to gangrenous bowel and a rise in resection rates and mortality [1, 3, 6, 7].
Congenital internal hernias are an atypical cause of small bowel obstruction, but this pathology should be considered in the diagnostic work-up of patients with acute onset of symptoms, who present with no palpable external hernias. A CT scan is helpful in diagnosing internal hernias, but the examination may still leave the surgeon uncertain in some cases. An operation is the only initiative that reveals the true cause of obstruction, emphasizing the importance of early laparotomy in avoiding ischaemia and necessity to resect.



