-
PDF
- Split View
-
Views
-
Cite
Cite
Steven N. Shephard, Sunday J. Lengmang, The missing foley catheter: an unusual finding in vesicouterine fistula, Journal of Surgical Case Reports, Volume 2013, Issue 12, December 2013, rjt115, https://doi.org/10.1093/jscr/rjt115
Close - Share Icon Share
Abstract
A 28-year-old G1P1 presented complaining of urine leakage per vaginum following caesarean delivery, accompanied by amenorrhoea, cyclic haematuria and cyclic pelvic pain. Examination findings were suggestive of vesicouterine fistula and the patient was taken for exploratory laparotomy, during which the foley catheter could not be identified within the bladder. During separation of the bladder from the uterus, the catheter was found to be traversing the fistulous tract into the uterine cavity. Vesicouterine fistula is a fairly uncommon type of urogenital fistula that is frequently associated with caesarean section. Surgical treatment remains the mainstay and successfully cured this patient.
INTRODUCTION
This report describes a case of vesicouterine fistula following caesarean delivery. Unique to this case, the foley catheter beats the odds and traversed the fistulous tract. We outline the presentation, identification and accepted management for surgical treatment of vesicouterine fistulas.
CASE REPORT
A 28-year-old G1P1 was referred to our fistula hospital with a 5-month history of leaking urine per vagina. The leakage was intermittent, and immediately followed caesarean delivery of a stillbirth after labouring 3 days. Additionally, she had 5 months of amenorrhoea but cyclic haematuria accompanied by cramping pains.
The genital examination was unremarkable, with no leakage of dye following retrograde filling of the bladder. Given her complaints, she was scheduled for an exploratory laparotomy for suspected vesicouterine fistula. A foley catheter passed immediately before surgery was noted to have no urine drainage, but the examination confirmed proper transurethral placement.
On surgical exploration, the bladder was identified, but the foley bulb was curiously absent. Dissecting the bladder completely free from the uterus revealed the problem. Surrounded by dense scar tissue was the missing foley catheter, traversing the fistulous tract (Fig. 1). Palpation of the uterus confirmed the inflated balloon was in the endometrial cavity.
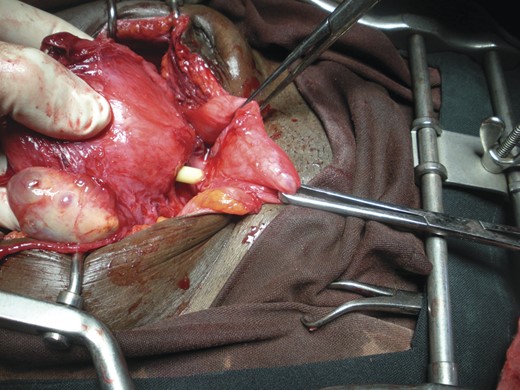
Vesicouterine catheter. Vesicouterine fistula clearly demonstrated the catheter found passing through the bladder (reflected to the right by Babcock clamps) to the uterus. Primary author's personal photograph.
DISCUSSION
Urogenital fistula continues to be a major problem in developing countries, primarily due to obstructed labour. In recent decades, however, there has been an increase in fistula cases resulting from caesarean section [1]. While most obstetric fistulas are vesicovaginal, this case highlights the vesicouterine type, one recognized to occur most often secondary to caesarean delivery [1–3]. Youssef [4] described a common presentation to vesicouterine fistula of amenorrhoea, cyclic haematuria (which he termed menouria) and urinary continence. Since then, case and series reports have demonstrated a variable presentation to this problem. Some report urinary incontinence, which is commonly intermittent, while others present with no urinary leakage. Similarly, cyclic haematuria also is sometimes present, but not always. It is believed that the passage of menses through the fistula is due to differences in the pressure gradients between the uterus and bladder, which also explains the lack of urinary leaking except when the pressure of the bladder is raised sufficiently, such as with micturition or Valsalva [5].
Surgical management is the mainstay of treatment for vesicouterine fistula, though some consider hormonal attempts using OCPs. Transperitoneal access to the fistula was employed in this picture, with dissection of the uterus from the bladder, closure of the uterine rent, then opening the bladder and repairing its fistula using a modified O'Connor technique. The follow-up at 3 and 10 months confirmed the resolution of this patient's symptoms. Similarly, published success rates for surgical management of this type of fistula are high [2].
CONFLICT OF INTEREST
The authors report no conflicts of interest. The authors attest to having obtained written consent from the patient whose case is reviewed in this report.



