-
PDF
- Split View
-
Views
-
Cite
Cite
Amir H. Lebastchi, Peter A. Prieto, Charlie Chen, Felix Y. Lui, Appendiceal endometriosis in a pregnant woman presenting with acute perforated appendicitis, Journal of Surgical Case Reports, Volume 2013, Issue 12, December 2013, rjt104, https://doi.org/10.1093/jscr/rjt104
Close - Share Icon Share
Abstract
Endometriosis is a common disease in women of childbearing age and is defined as the presence of endometrial glands and stroma in organs outside of the uterine cavity. Appendiceal endometriosis is very uncommon and accounts for a small fraction of all cases of extrapelvic endometriosis. Cases of that which occur during pregnancy are extremely rare with an incidence that ranges between 3 and 8 deliveries per 10 000. This makes the diagnosis extremely difficult and represents a challenge in the management of the patient. In this report we describe the case of a pregnant woman who underwent ileocecectomy for perforated appendicitis stemming from endometriosis and subsequent pre-term delivery of a 31-week-old fetus.
INTRODUCTION
The presence of ectopic endometrial tissue outside the lining of the uterine cavity defines endometriosis [1]. While it is a common disorder in women of reproductive age, manifestations in the appendix are exceedingly rare and difficult to diagnose due to unusual symptomatology and low prevalence of the disease. Definitive diagnosis is confirmed on postoperative histologic examination, which may represent a challenge in pregnant patients. While surgery poses a risk for mother and fetus [2] delays in diagnosis and complications from appendicitis can lead to devastating outcomes for both [3, 4]. Here, we describe the case of a 33-year-old woman, who was 31 weeks pregnant, who underwent a right ileocecectomy for an acute perforated appendicitis secondary to appendiceal base endometriosis.
CASE REPORT
A 33-year-old female patient at 31 weeks of gestation presented to our emergency department complaining of sharp constant upper abdominal pain that had grown progressively worse over the preceding 24 h period. She denied fever, chills, changes in her appetite, nausea or vomiting. Her past medical history was significant for unspecified inflammatory bowel disease and chronic urinary tract infections. She was confirmed by ultrasound to have a 31-week intrauterine pregnancy that until presentation had been largely uneventful. She was admitted to the maternal–fetal medicine service and was found to have a white blood cell count of 18.700/mm3 with 87% neutrophils and frequent contractions. The obstetricians administered Mg2+ for tocolysis and steroids for fetal pulmonary maturation, and the patient underwent an amniocentesis that was negative for chorioamnionitis. Her urinalysis was unremarkable and urine culture was sent and her workup had been otherwise unrevealing including ultrasound imaging of the right upper quadrant, which did not show any pertinent biliary pathology.
The patient underwent an MRI, which demonstrated a single fetus in cephalic vertex position, but could not completely visualize the appendix and was negative for inflammatory changes in the right lower quadrant or surrounding the terminal ileum. Initially, the patient improved clinically, however over the following 2 days her severe upper abdominal pain returned. A repeat MRI was obtained that now showed no appendix, but a multilobulated cystic mass complicated with an abscess measuring up to 13 mm and free fluid tracking along the right paracolic gutter and a small amount of perihepatic free fluid (Fig. 1). Interestingly, the study also showed small rounded hypodensities in the base of the cecum that were initially interpreted as fecalith or intraluminal gas, but in retrospect might have presented ectopic endometrial glands. These findings in conjunction with her rising white blood count (21 000/mm3) and worsening physical examination were concerning for an acute perforated appendicitis and the patient was brought to the operating room for an open appendectomy in the presence of the obstetric team for fetal monitoring. Upon entering the abdomen abundant free fluid and a grossly inflamed, necrotic and perforated appendix were noted. Frozen section of the tissue came back as grossly inflamed perforated appendicitis and transmural intestinal endometriosis with extensive dezidualization (Fig. 1). Given the extensive nature of the perforation, likely secondary to endometriosis at the base of the appendix, an ileocecetomy was performed. The patient tolerated the patient well and fetal monitoring did not show any signs of distress at the conclusion of the case.
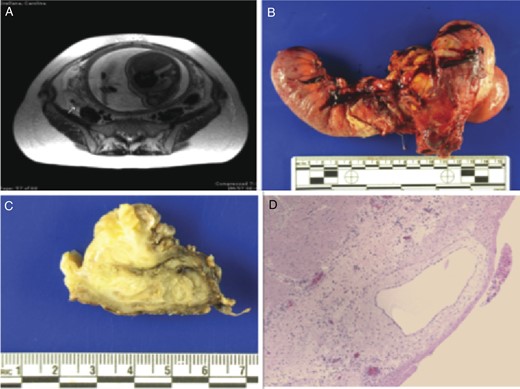
Radiographic and pathologic findings of appendicular endometriosis presenting as acute appendicitis in a gravid patient. (A) Abdominal MRI showing an enlarged appendix with intraluminal hypodensities representing ectopic endometrial tissue and periappendiceal inflammatory changes (arrow) in a gravid patient. (B) Gross pathology of distal ileum, cecum and adherent appendix. The appendix is encased in fibrous adhesions and hemorrhage marking the extent of the inflammatory process. The cecum has a perforation in the region of the appendiceal base (C) Formalin-fixed ileum and appendix. The light yellow area illustrates ectopic endometrial tissue. (D) Histology of the resected appendix depicts transmural intestinal endometriosis with extensive decidualization. This interpretation was supported by immunostains for CD68 and cytokeratin AE1/AE3 (not shown).
Approximately 5 h postoperatively the patient experienced painful contractions and fetal heart monitoring showed late decelerations. Pelvic examination showed an 8-cm dilated cervix. Subsequently the patient's membranes ruptured and she delivered a viable male infant who required 36 h of mechanical ventilation and newborn special care unit (NBSCU) admission. The patient made a full recovery in a few days and the infant did well in the NBSCU.
DISCUSSION
Endometriosis is a common gynecological disease in reproductive-aged women and can affect the appendix. A review of the literature estimated the prevalence of appendiceal endometriosis to be 2.8% in patients diagnosed with endometriosis and 0.4% among the general population [5]. The incidence involving the appendix is reported to be just <1% of the total endometriosis cases. Endometriosis that presents as acute appendicitis during pregnancy is very uncommon and ranges between 3 and 8 deliveries per 10 000 [6] and there have been to date only four reported occurrences of perforated appendicitis secondary to appendiceal endometriosis [7–9].
Our case presents multiple clinical challenges. The presenting symptoms of the patient—sharp right upper quadrant pain in the absence of constitutional symptoms—are unusual findings in acute appendicitis and may have delayed an early diagnosis as this pain was initially diagnosed with pregnancy-related cramping abdominal pain. Early diagnosis was further complicated by the fact that the patient was in her third trimester, where certain physiologic and anatomic changes related to the gravid state, such as an elevated white blood cell count and the upward displacement of the appendix by the uterus need to be taken into account. The low prevalence in association with non-pathognomonic clinically and laboratory findings makes the preoperative diagnosis very difficult and a delayed detection almost inevitable, which harbors a risk for perforation, peritonitis, abscess formation and fetal risk. Unfortunately, the occurrence of these complications is higher with endometriosis-related acute appendicitis as decidual cells are affected by hormonal changes in pregnancy. Intra-appendiceal decidual reactions induce an inflammatory response, which, in turn, increases the risk of perforation [3]. This is crucial as perforation of the appendix is associated with an increased overall morbidity and mortality of both infant and mother [3, 4].
Despite the delayed diagnosis and subsequent surgical intervention, in this case an elaborated multidisciplinary approach can achieve good outcomes even in complicated cases. The goal of surgical treatment of intestinal endometriosis is to remove the disease and to restore continuity and function. The extent of the resection is determined by intraoperative inspection, which usually results in accurate diagnosis of endometriosis. Postoperative gynecological assessment and follow-up are mandatory for intestinal endometriosis to avoid further complications associated with this disease.
Endometriosis of the appendix is rare and very difficult to diagnose preoperatively. However, our case report alerts physicians that acute appendicitis very frequently presents with atypical clinical and laboratory findings, but should always be included in the differential diagnosis of acute abdominal pain in pregnant women. Early intervention is strongly recommended, as any delay in surgical intervention may increase the chance of perforation and peritonitis, which poses mother and fetus in great risk, especially during the last trimester of pregnancy.



