-
PDF
- Split View
-
Views
-
Cite
Cite
Polikseni Eksarko, Sharique Nazir, Edmund Kessler, Patrick LeBlanc, Michael Zeidman, Armand P. Asarian, Philip Xiao, Peter J. Pappas, Duodenal web associated with malrotation and review of literature, Journal of Surgical Case Reports, Volume 2013, Issue 12, December 2013, rjt110, https://doi.org/10.1093/jscr/rjt110
Close - Share Icon Share
Abstract
Intestinal obstruction due to midgut malrotation in neonates is well known. The incidence of malrotation in newborns is around 1:500 and the symptomatic incidence is 1:6000 births. Duodenal web as a cause of intestinal obstruction is less common and is reported to be 1:10 000–1:40 000. Malrotation is known to be associated with other congenital obstructive anomalies including duodenal atresia, stenosis and duodenal web. But, intestinal obstruction due to malrotation associated with duodenal web has been reported only rarely with a few published cases in our literature review. We present a case of intestinal obstruction diagnosed in the prenatal period via sonogram. A plain X-ray of the abdomen after birth showed a distended duodenum with paucity of air distally suggesting duodenal obstruction. An exploratory laparotomy showed a duodenal web proximal to the sphincter of oddi. The patient also had an associated malrotation and underwent Ladd's procedure and appendectomy. The post-operative period was uneventful.
INTRODUCTION
Intestinal obstruction due to midgut malrotation in newborns is well known. The incidence of malrotation is ∼1:500 births and the symptomatic incidence is 1:6000 [1, 2]. The incidence of duodenal web as a cause of intestinal obstruction is 1:10 000–1:40 000 [3]. However, intestinal obstruction due to malrotation associated with doudenal web is rare.
CASE REPORT
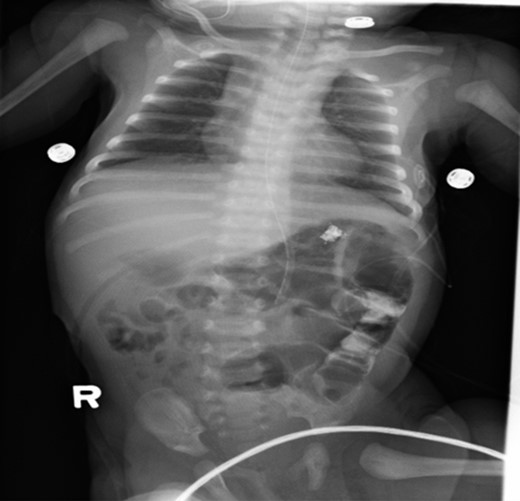
A 1-day-old baby girl, born by normal spontaneous vaginal delivery, was evaluated for abdominal distension and history of having not passed meconium. An abdominal X-ray was suspicious for malrotation (Fig. 1). The patient did not have any evidence of sepsis. An echocardiogram ruled out any congenital cardiac anomalies.

Pre-operative abdominal x-ray showing a gastric and duodenum distention with paucity of small bowel gas distally, suggesting duodenal atresia and malrotation.
The patient underwent an exploratory laparotomy; findings demonstrated a distended duodenum with cecum and appendix at the left upper quadrant fixed by Ladd's bands. The contents of the stomach could not be milked down distally. A duodenotomy incision identified a large duodenal web with a blind pouch (Fig. 2). Distal to the web, the duodenum had normal caliber lumen. The duodenal web was resected and the duodenotomy was closed primarily. The cecum was positioned in the left upper quadrant. An appendectomy was performed and the abdomen closed primarily.
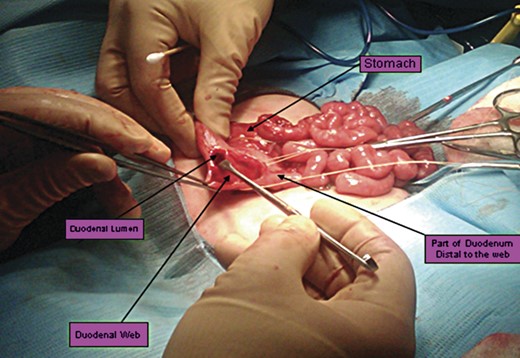
Intra-operative picture showing a duodenotomy incision that reveals a duodoneal web (marked by arrow).
Postoperative care included monitoring in neonatal intensive care unit. Upper GI series (Figs 3 and 4) demonstrated no evidence of leakage. The patient tolerated a trial of pedialyte feedings and was subsequently discharged home.
Post-operative abdominal x-ray showing gas throughout the bowel and residual contrast in the descending colon.

Microscopic examination showing a normal portion of duodenum with a full thickness of the wall and duodenal web lacking the muscularis propria layer.
DISCUSSION
Lesions that cause congenital duodenal obstruction are classified as either intrinsic or extrinsic. The intrinsic causes include duodenal stenosis, atresia or web. The extrinsic causes include malrotation with Ladd's bands, annular pancreas, anterior portal vein and duodenal duplication [4]. Our case is unusual in that both intrinsic and extrinsic causes of obstruction were present: duodenal web and malrotation with Ladd's bands.
As the bowel develops in the fetus, it migrates out of the abdominal wall through the umbilical cord to receive nutrition [1]. This happens around Week 6 of gestation. Between weeks 7 and 10, the bowel begins to return to the abdominal cavity and initiates a two-step rotation process, rotating a total of 270° counterclockwise around the superior mesenteric artery (SMA) [1, 2]. When the rotation process is complete, the ligament of Treitz fixes the mesentery to the retroperitonium, preventing the mesentery from twisting upon itself [1, 2].
Intestinal malrotation is an aberration of this embryologic process. This pathology lies on a spectrum of complete non-rotation to abnormal rotation [2]. Any deviation from a normal intestinal rotation affects the process of fixation. Furthermore, congenital bands of fibrous tissue that attempt to fix the malrotated bowel can compress underlying bowel and cause obstruction [1, 2]. These are called Ladd's bands, named after the ‘father of pediatric surgery’, William Ladd [5]. In our case the degree of obstruction of duodenum seemed out of proportion, prompting to exploration of the duodenum, which revealed the web.
Malrotation is distributed equally amongst males and females [1, 6]. Risk factors include low birth weight, toxic injury and young maternal age [6]. Eighty percent of all cases present by the first month of life [2]. Other congenital malformations such as abdominal wall defects and diaphragmatic hernias are concomitant with intestinal malrotation 70% of the time [1, 6, 7].
The most common sign of malrotation is bilious vomiting. Malrotation is an emergent situation that must be ruled out when newborns have bilious emesis [1, 2]. Other symptoms include drawing up of legs to alleviate abdominal cramps, tachycardia, tachypnea and failure to pass meconium.
The gold standard in the diagnosis of intestinal malrotation is an upper gastrointestinal series [1]. A non-pathologic UGIS would demonstrate the ligament of Treitz just left of the midline at the level of the gastroduodenal junction [1]. Any deviation of the ligament of Treitz from this location is diagnostic for malrotation. If the UGIS is indeterminate, a contrast barium enema study helps define the location of the cecum [1, 5]. A contrast BE used to be the gold standard; however, it has been replaced because 20–40% of confirmed cases of malrotation have a normal cecal position [8, 9]. Ultrasound is used to detect malrotation. The ‘whirlpool’ sign, referring to the appearance of the SMV wrapping in a clockwise manner around the SMA, has been used as evidence for malrotation [9]. Although sonography is the least invasive imaging modality with minimal radiation exposure, the sensitivity and specificity compared with UGIS is low, and thus, UGIS is still the gold standard [9].
The treatment of choice for intestinal malrotation is the Ladd's procedure, first performed in 1932 by William Ladd [1, 8]. This procedure can be performed either open or laparoscopic, with similar outcomes [7]. The surgeon untwists the mesentery, divides any Ladd's bands and positions the small bowel on the right side of the abdominal cavity and the large bowel on the left [1]. It is recommended to perform an appendectomy, because appendicitis on the left side can easily lead to misdiagnosis [1, 8]. Although the Ladd's procedure is effective in alleviating bowel obstruction, complications following the procedure are seen in 46% of patients, more than half of which require further surgery [8]. Common complications include small bowel obstruction and short-bowel syndrome [8].
During Weeks 4–6 of gestation, the epithelium of the bowel rapidly proliferates, obliterating the lumen [4]. The lumen then recanalizes at Week 12. If this recanalization does not occur, the result can manifest as any of the intrinsic causes of congenital duodenal obstruction: stenosis, atresia or web [4].
Duodenal web occurs in 1 out of 10 000–40 000 births [3]. The failure of recanalization leaves behind a thin web with mucosa and submucosa layers only; the muscular layer is absent [3]. With a high amount of pressure proximal to the obstruction, peristalsis can cause the web to balloon distally, taking on the form of a wind sock [3, 10]. This windsock sign can be visualized on sonography, UGI series and endoscopy [10].
Symptoms of duodenal web are similar to those of malrotation, with projectile bilious vomiting being the most common. Surgical resection has been the foundation of treatment; however; endoscopic techniques are showing similar efficacy without the burden of having surgical intervention [3].



