-
PDF
- Split View
-
Views
-
Cite
Cite
Shaheel M. Sahebally, Rishabh Sehgal, Justin Kelly, Peter N. Faul, David Waldron, Metastatic breast cancer presenting as a gallstone ileus, Journal of Surgical Case Reports, Volume 2013, Issue 12, December 2013, rjt113, https://doi.org/10.1093/jscr/rjt113
Close - Share Icon Share
Abstract
Metastatic breast cancer to the small bowel (SB) presenting as gallstone ileus and resulting in SB obstruction has not been described previously. A 76-year-old woman with previous metastatic breast cancer to the axial spine and hips presented with abdominal pain and bilious vomiting. CT scanning revealed SB obstruction consistent with gallstone ileus. The patient underwent two segmental SB resections for distal ileal strictures mimicking what appeared to be macroscopic Crohn's disease. The entero-biliary fistula was undisturbed. Pathological analysis revealed the dual pathologies of gallstone ileus and metastatic carcinoma from a breast primary causing luminal SB obstruction. Improvements in staging and treatment modalities have contributed to the increased overall long-term survival for breast cancer, compelling clinicians to consider metastatic breast cancer as a differential diagnosis in women presenting with new onset of gastrointestinal symptoms in order that appropriate treatment be administered in a timely fashion.
INTRODUCTION
Breast cancer is the second leading cause of cancer-related mortality in women [1]. Metastatic breast cancer to the gastrointestinal tract (GIT) is unusual. Although lobular type breast carcinoma is less common compared with ductal type carcinoma, it has a higher propensity to metastasize to the GIT [2]. With improved longevity of breast cancer patients owing to improved therapeutic regimens, unusual presentations of metastatic disease are being encountered.
Gallstone ileus, on the other hand, accounts for <1% of all cases of mechanical bowel obstruction and mainly affects the elderly population (>70%) [3]. We report a case of small bowel obstruction caused by an obstructing gallstone in small bowel strictured by metastatic breast cancer.
CASE REPORT
A 76-year-old Caucasian woman was admitted with a 2-week history of intermittent colicky lower abdominal pain associated with bilious vomiting and mild abdominal distension. She was previously diagnosed with left breast cancer 18 years ago for which she had undergone an oncological wide local excision, focused external beam radiotherapy and adjuvant treatment with tamoxifen for 5 years. Unfortunately, she developed regional recurrence with bony metastases 17 years following her original diagnosis. She was treated with palliative chemoradiotherapy and had an excellent response to treatment.
Physical examination revealed an elderly lady with stable vital signs. The abdomen was mildly distended with tenderness and guarding noted in the peri-umbilical region. Laboratory investigations, including haematological, biochemical, inflammatory and coagulation profiles, were all within normal limits.
A plain abdominal radiograph was also unrevealing. She proceeded to have computerized tomography (CT) scan of her abdomen and pelvis, which showed dilated small bowel loops consistent with small bowel obstruction. There were two filling defects noted, one in her proximal ileum suspicious for a non-calcified gallstone and the second distally in her terminal ileum (Figs 1 and 2). Appearances were suggestive of gallstone ileus. She was adequately resuscitated and underwent a laparotomy. The small bowel was narrowed in two segments: proximally secondary to an impacted gallstone and an area of stricturing noted distally. Both segments were resected with end-to-end anastomosis performed in a two-layer standard hand-sewn fashion. The clinical impression was one of dual pathology including Crohn's disease and gallstone ileus. She did not undergo a cholecystectomy or repair of her cholecystoduodenal fistula. She made an uneventful post-operative recovery and was discharged home well on Day 7.
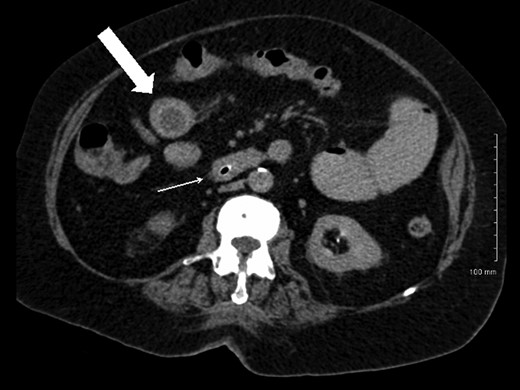
Axial CT image demonstrating gallstone in proximal ileum (block arrow) and distal ileal luminal narrowing (thin arrow).
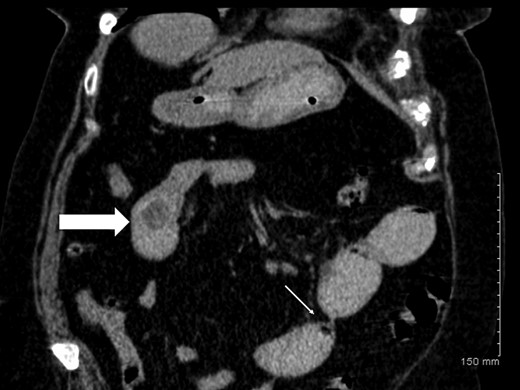
Coronal CT image demonstrating gallstone ileus (block arrow) and stricture in distal ileum (thin arrow).
Histopathological examination of the resected specimens showed a 3-cm intraluminal gallstone within the proximal ileum, with focal metastatic carcinoma consistent with breast primary present in the adjacent mesenteric adipose tissue (Fig. 3), while the more distal, strictured ileal segment revealed mucosal and transmural involvement by metastatic breast carcinoma (Fig. 4). The tumour cells were strongly positive for cytokeratin, oestrogen receptor and focal progesterone receptor (<5%), consistent with metastatic breast carcinoma. They also displayed a mixed ductal and lobular differentiation pattern.
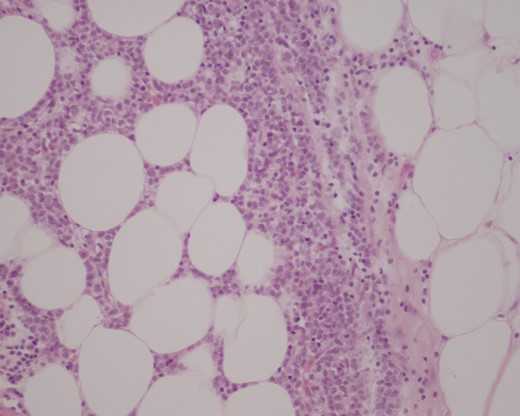
Haematoxylin and eosin (H&E) stain of proximal ileum showing focal metastatic breast carcinoma in mesenteric tissue (medium power field).
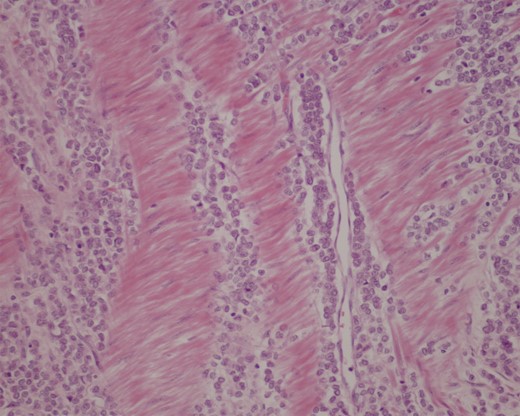
Immunohistochemical stain of distal ileal resection showing an extensive transmural involvement by metastatic carcinoma (×200).
DISCUSSION
A minority (10%) of patients with breast cancer develops distant metastases to the liver, lungs, bone and brain despite undergoing surgical excision and medical oncologic therapies [4]. Metastases to the bowel in general are relatively rare; however, when present classically originate in the setting of malignant melanoma, colon cancer, ovarian or cervical cancer [5, 6]. Breast cancer metastases to the bowel however are extremely uncommon. Metastatic small bowel disease can present with a variety of non-specific symptoms, and often masquerades as other commoner gastrointestinal disorders [6, 7].
The terminal ileum is the commonest site involved in gastrointestinal spread from breast cancer, followed by the proximal small bowel. Clinical findings may mimic Crohn's disease, as reflected in our case. Despite invasive ductal breast carcinoma being the more prevalent subtype in women (90%), invasive lobular carcinoma has a higher propensity to spread to the small bowel, accounting for 54% of all gastrointestinal metastasis in one series [4].
Gallstone ileus is a rare but severe complication of cholelithiasis. The most frequent sites for impaction include the terminal ileum and ileocaecal valve (50–75%), followed by the proximal ileum and jejunum (20–40%), stomach and duodenum (10%) [8]. Diagnosis may be delayed as only 10% of gallstones are adequately calcified to enable radiological detection [9]. The optimal management of gallstone ileus is still the subject of ongoing debate [3]. While a one-stage procedure consisting of enterolithotomy, cholecystectomy and fistula repair is the mainstay in non-high-risk patients, it carries a high incidence of complications in the severely comorbid. [8]. Other surgical options include an enterolithotomy alone, or an enterolithotomy followed by an interval cholecystectomy (two-stage procedure) [3]. It is also prudent to note that an entero-biliary fistula can be successfully managed conservatively and spontaneous closure has been reported in more than 50% of cases [10].
Our case is different from the reported literature in that small bowel obstruction was triggered by the dual pathologies and synchronous presentations of metastatic breast carcinoma causing a gallstone ileus. To the best of our knowledge, this is the first case report describing metastatic breast carcinoma to the small bowel presenting as a gallstone ileus.
CONCLUSIONS
Metastatic breast cancer involving the small bowel can mimic other more common gastrointestinal pathologies and it is vital to bear this in mind when considering the differential diagnosis in women with a history of breast cancer who present with new onset of gastrointestinal symptoms.
CONFLICT OF INTEREST
Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal. The authors declare that they have no competing interests.



