-
PDF
- Split View
-
Views
-
Cite
Cite
Zachary Bauman, John Lim, Pneumoperitoneum as a result of a ruptured splenic abscess, Journal of Surgical Case Reports, Volume 2013, Issue 12, December 2013, rjt111, https://doi.org/10.1093/jscr/rjt111
Close - Share Icon Share
Abstract
We encountered a case of ruptured splenic abscess presenting as peritonitis and pneumoperitoneum. Our patient did not have an underlying neoplasm nor was she immunosuppressed. In our case, splenectomy was the treatment of choice in combination with antibiotics, which proved to be a good outcome for the patient. Work-up for the cause of the abscess was negative, although bacteria predominately found in the oral flora were isolated from the abscess. We strongly encourage that splenic abscess be considered on the differential diagnosis of patients presenting with pneumoperitoneum and peritonitis, although a clinical rarity.
INTRODUCTION
The incidence of splenic abscess is a clinically uncommon disease with current literature reporting a 0.14–0.7% occurrence rate [1, 2]. Although splenic abscesses are a clinical rarity, they have the potential to be fatal. The presentation of this disease is often vague and insidious including left upper quadrant abdominal pain, fever and chills [2]. Additionally, these patients may present with leukocytosis, left upper quadrant mass and pleural effusion on chest X-ray [1]. Splenic abscesses generally occur in patients with underlying comorbidities, which commonly include neoplasia, immunodeficiency, trauma, metastatic infection, splenic infarct or diabetes [2]. The best management of splenic abscesses is still debatable with the various modalities including antibiotics, percutaneous drainage or splenectomy. The current literature supports a 67–100% success rate with percutaneous drainage [2]; however, Tung et al. [1] states that the most optimal treatment for splenic abscess is splenectomy.
Of the 600 cases of splenic abscess documented in the current literature, most have been described as air confined to the left upper quadrant on chest X-ray [3]. We report a young patient with a ruptured splenic abscess resulting in an acute abdomen and pneumoperitoneum. To our knowledge, there have only been four other reported cases of ruptured splenic abscess causing pneumoperitoneum [3, 4].
CASE REPORT
A 48-year-old female with the past medical history of diabetes, coronary artery disease and psoriasis, presented with acute onset of diffuse abdominal pain 2 days prior to admission to the hospital. Upon presentation, she was tachycardic with a heart rate of 130 and hypotensive with a blood pressure of 78/45. The patient was afebrile and alert and oriented to person, place and time. She was resuscitated in the emergency department with intravenous fluids and her blood pressure and heart rate responded appropriately.
Her initial labs showed a normal WBC level of 8.3 thou/mcL; however, the patient was acidotic with a pH of 7.29 and a lactic acid level of 3.5 mmol/l. An acute abdominal series was obtained demonstrating free air below the right hemidiaphragm (Fig. 1). Physical examination showed a distended abdomen with tenderness, guarding and signs of peritonitis. The patient was subsequently boarded for an exploratory laparotomy with repair of perforated viscus, as that is the usual cause of pneumoperitoneum, especially under the right hemidiaphragm. Because the patient's vital signs stabilized after being resuscitated, the decision was made to obtain a CT scan to better assess the location of the perforated viscus. Much to our surprise, the patient did not have a perforated viscus, but a splenic abscess that had ruptured causing the pneumoperitoneum (Fig. 2).
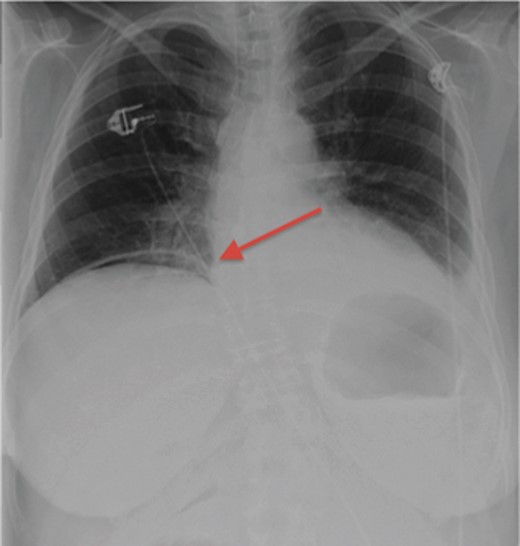
Acute abdominal series demonstrating free air under the right hemidiaphragm.
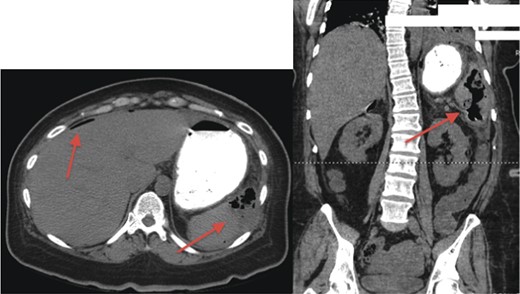
CT scan demonstrating gas-forming splenic abscess and free air in the peritoneal cavity.
The patient then became increasingly confused and her vital signs again deteriorated demonstrating worsening sepsis. The patient was taken to the operating room where a laparoscopic splenectomy was attempted but was quickly converted to laparotomy with splenectomy due to the gross contamination of the abdomen. The abdominal compartment was copiously irrigated and the abdomen was closed. The surgery was without any complications. The patient was continued on antibiotics and taken to the intensive care unit for post-operative care.
The patient did well post-operatively. The splenic abscess grew Prevotella intermedia, a bacterium commonly found in the oral flora. Her blood cultures were negative. The patient underwent a full work-up looking for the source of the splenic abscess. A transesophageal echocardiogram was performed but was negative for any masses, thrombus or vegetation. Furthermore, a panorex was performed and was negative as the patient had reported tooth pain 1 week prior to her admission. The patient was finally deemed stable for discharge on post-operative day 10. She returned to the clinic on post-operative day 14 to receive her splenectomy vaccinations.
DISCUSSION
Although a rare disease, splenic abscess should be included on the differential diagnosis of a patient presenting to the hospital with peritonitis or pneumoperitoneum. This is especially true for patients who are immunocompromised or have underlying comorbidities including neoplasia, diabetes, trauma or history of splenic infarct or embolization [2].
In our case, CT scan provided important information about the cause of our patient's pneumoperitoneum, as we had assumed it was due to a perforated ulcer or diverticulitis. This did change our operative management, as we attempted to perform a less invasive surgery on our patient by starting with a laparoscopic technique. However, we had to convert to an open splenectomy due to the gross contamination and adhesions from the splenic abscess. In retrospect, an open laparotomy was the best approach to this patient's care as it allowed for better visualization and irrigation of the abdominal cavity. It is unknown if we had successfully performed the splenectomy laparoscopically if it would have decreased recovery time. The current literature supports the laparoscopic splenectomy as a safe and effective procedure in patients with splenic abscess demonstrating an average length of stay of 14 days [5]. In our case, the patient remained in the hospital for only 10 days after converting to the open procedure.
The current literature reports that the most common organisms found in splenic abscesses are aerobic microbes, particularly Streptococci and Escherichia coli [2]. In our case, the microorganism isolated was the anerobe Prevotella intermedia. This microbe is commonly found in the oral flora and is associated with periodontal disease. Although our transesophageal echocardiogram and panorex were both negative, we believe this splenic abscess developed as a result of translocation of the oral flora as the patient was complaining of a tooth ache 1 week prior to her presentation.
In summary, we have presented a case of ruptured splenic abscess as a cause of pneumoperitoneum and peritonitis. Although rare, we encourage splenic abscess be included on the differential diagnosis of patients presenting with peritonitis and pneumoperitoneum. Although there is still controversy in the current literature when managing splenic abscesses, our recommendation is splenectomy, especially in the case of ruptured splenic abscess resulting in hemodynamic instability. Whether it is better to perform the splenectomy laparoscopically or open is still debatable, the important thing is to obtain source control. Furthermore, a full work-up is required for patients presenting with a splenic abscess as the underlying cause could cause more serious illnesses for the patient in the future.
CONFLICT OF INTEREST
There are no conflicts of interests or financial funding to disclose for any of the contributing authors.



