-
PDF
- Split View
-
Views
-
Cite
Cite
L.S. Alder, G. Elver, F.J. Foo, M. Dobson, Giant rectal gastrointestinal stromal tumours: a diagnostic and therapeutic challenge, Journal of Surgical Case Reports, Volume 2013, Issue 12, December 2013, rjt103, https://doi.org/10.1093/jscr/rjt103
Close - Share Icon Share
Abstract
Gastrointestinal stromal tumour (GIST are the most common mesenchymal tumours; however, rectal GISTs account for <5%. In the pelvis they represent a diagnostic challenge with giant GISTs likely to be malignant. They may present with urological, gynaecological or rectal symptoms. Sphincter-preserving surgery can be aided by neoadjuvant therapy. We present an uncommon case of giant rectal GIST masquerading as acute urinary retention.
INTRODUCTION
Gastrointestinal stromal tumours (GISTs) are the most common mesenchymal neoplasms arising in the gastrointestinal tract. However, rectal GISTs only account for 5% of GISTs, whilst stomach and small bowel account for 80–95% [1].
Complete surgical resection remains the optimal treatment in primary localized lesion [2, 3]. For recurrent, metastatic GISTs or unresectable tumours the treatment of choice is tyrosine kinase inhibitors [3]. In rectal GISTs even extensive abdominoperioneal resection with radical clearance has shown significant locoregional recurrence [2]. Presentation of these large pelvic tumours remains a diagnostic challenge for all involved in pelvic surgery. We describe a case of a locally advanced GIST situated in the rectum, presenting under urology, treated by neoadjuvant imatinib mesylate followed by radical surgery.
CASE REPORT
An elderly man in his seventies presented to the Urology department with two episodes of acute urinary retention. There were no rectal symptoms and rectal examination revealed an enlarged prostate. He underwent a laser transurethral resection of prostate during which a large palpable pelvic mass was noted. The subsequent urgent MR pelvis revealed a large tumour in the mesorectum arising from the anterior rectum 10 × 8.5 cm (Figs 1 and 2). A transrectal ultrasound and biopsy were performed; histology revealed a spindle cell tumour, with positive immunostains for CD117 and DOG1 with 5 mitoses per 50 high power fields. This was confirmed to be a locally advanced high-risk GIST.
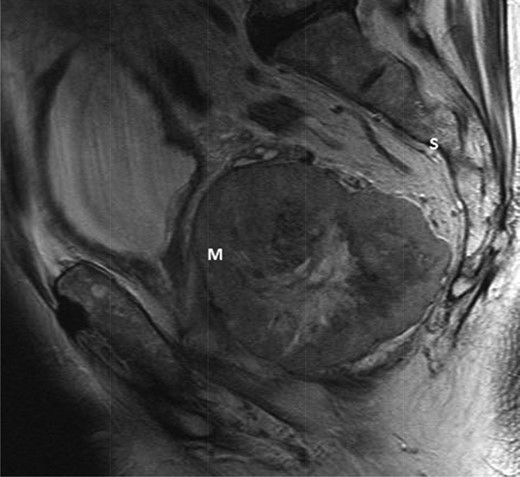
T2-weighted sagittal image demonstrating a large mass (m) anterior to the sacrum (S) and posterior to the bladder.
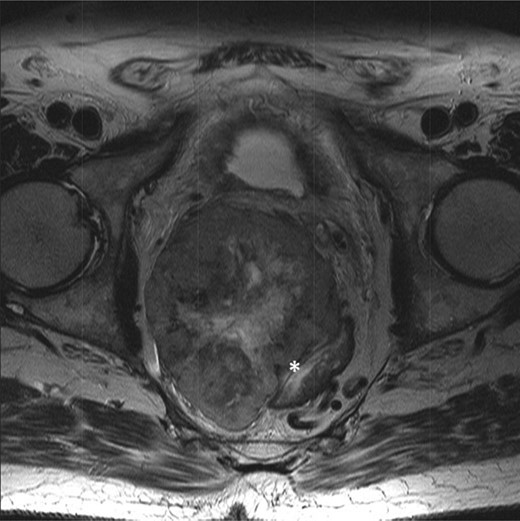
T2-weighted axial showing the same mass lying adjacent to the anterior wall of the rectum (*).
The multidisciplinary team review advised neoadjuvant treatment with imatinib mesylate and further reassessment. Repeat MR pelvis and staging PET CT abdomen, thorax and pelvis were then performed. These showed a large extra-luminal tumour with downsizing in tumour bulk (6 × 5.7 × 5.4 cm) (Figs 3–5) but in close approximation with the right seminal vesicle.

Axial fused PET-CT image pre-treatment, demonstrating that the mass has avid peripheral tracer uptake and a hypometabolic, tracer inavid centre.
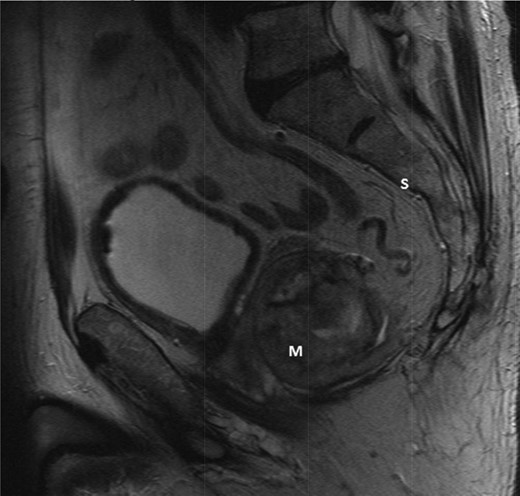
T2-weighted sagittal images after 3 months of imatinib mesylate therapy. The mass has shown a significant reduction in size (Mass = m, Sacrum = s).

T2-weighted axial images after 3 months of imatinib mesylate therapy. The mass has shown a significant reduction in size (white star).
Further examination under anaesthesia, flexible sigmoidoscopy and cystoscopy were performed. The tumour was a large right-sided mass with no prostatic involvement. An elective Hartmann's procedure plus possible pelvic clearance was organized. Intraoperatively a large tumour in close proximity to the posterior bladder and seminal vesicles was found. Although there was no evidence of invasion, dissection of the plane between the GIST and posterior bladder was not possible, thus cystectomy and prostatectomy were performed with an ileal conduit and urostomy. The sigmoid colon and rectum were resected leaving an end colostomy as planned. In the postoperative period the patient developed signs of sepsis. A subsequent CT revealed an anastomotic leak at the ileo-ileal site. The patient returned to theatre, the anastomosis was taken down and a double barrel ileostomy sited. He initially went on to recover well. Operative histology revealed reduced mitotic activity and downgrading of tumour activity with clear R0 resection margins.
DISCUSSION
GISTs arise from the interstitial cells of Cajal, and over 90% of these tumours demonstrate a mutation in the tyrosine kinase proto-oncogene, CD117(c-kit) [1]. Diagnosis is dependent on the morphology of either spindle cell or epitheloid, and immunohistological identification of CD117 and CD34 [1, 2].
Colorectal GISTs can present with perianal pain, bleeding or obstruction. Incidental diagnosis during per rectal or endoscopic examination has been reported in a few cases [1, 2]. Less commonly they present following urological investigation [1, 2].
Locoregional lymphatic spread is extremely rare, and local spread of the tumour tends to displace adjacent organs rather than invade tissue [1, 2, 4]. Over 70% of GISTs present with a tumour over 5 cm in diameter, with those over 10 cm having a poor 5-year prognosis [2].
Curative surgery (R0) is associated with an optimal outcome in those with localized primary disease [1, 2]. Rectal GISTs can demonstrate close proximity to the pelvic floor, and are often of large size, therefore representing a challenge for sphincter preserving surgery [2]. The most common surgical resections include anterior and abdominoperineal resection, although mesorectal clearance is not usually required due to unlikely lymphatic invasion.
For those with metastatic disease, tumours deemed inappropriate for resection or recurrent disease tyrosine kinase inhibitors (imatinib mesylate) are an alternative treatment [3, 4].
Primary GISTs >5 cm may benefit from 8 to 12 weeks of neoadjuvant treatment prior to surgery with no adverse effect [3]. Given the rarity of rectal GISTs this may help to improve sphincter-preserving surgery in giant (>10 cm) rectal GISTs. Neoadjuvant treatment prior to surgical resection in primary locally advanced GISTs show an improved overall survival and progression-free survival [3]. This benefit is more apparent in high-risk ‘giant’ GISTs >10 cm for downsizing of tumour and hence a less aggressive surgery which is most apparent with pelvic presentations. Neoadjuvant therapy may help to improve resectability of the tumours; this is particularly important in the confines of the pelvis. However, we only depict one case and treatment option. Similar cases would need a tailored multidisciplinary approach to investigation and treatment. It highlights the importance of understanding alternative pelvic pathology amongst a range of specialities.
ACKNOWLEDGEMENTS
Many thanks to Mr Nigel Scott for clinical guidance with regard to this complex case and the Royal Preston Hospital Colorectal department for their advice on this case.



