-
PDF
- Split View
-
Views
-
Cite
Cite
Noora Al Shahwani, Parkash Mandhan, Abdelrahman Elkadhi, Mansour J. Ali, Abdel Latif, Congenital duodenal obstruction associated with Down's syndrome presenting with hematemesis, Journal of Surgical Case Reports, Volume 2013, Issue 12, December 2013, rjt108, https://doi.org/10.1093/jscr/rjt108
Close - Share Icon Share
Abstract
Congenital duodenal obstruction is usually characterized by onset of early vomiting due to high bowel obstruction. Presentation of congenital duodenal obstruction with acute gastrointestinal bleeding is very uncommon. We present an unusual case of congenital intrinsic duodenal obstruction associated with the Down's syndrome presenting with hematemesis secondary to duodenitis. This is a rare presentation of congenital duodenal obstruction associated with Down's syndrome in addition to seven cases previously reported in the English literature.
INTRODUCTION
Congenital duodenal obstruction is one of the more common intestinal anomalies encountered by pediatric surgeons, occurring in 1 in 2500–5000 live births. In 25–40% of patients, it is associated with trisomy 21, and 5% of patients with trisomy 21 have duodenal atresia [1, 2]. About two-thirds of all congenital duodenal obstructions are congenital intrinsic duodenal obstructions (CIDO) [2, 3], a condition characterized by the onset of bilious vomiting within 24 h of birth. CIDO accompanied by acute gastrointestinal bleeding is very uncommon and may lead to suspicion of malrotation with mid-gut volvulus. We describe a patient with CIDO associated with Down's syndrome, who presented with hematemesis on Day 2 of life. To our knowledge, only seven patients with this condition have been described previously in the English language literature.
CASE REPORT
A 2-day-old girl was referred to our service with sudden onset of severe hematemesis. Prenatal history was significant for intrauterine growth retardation. She was born at the gestational age of 37/40 with a birth weight of 2.1 kg. On examination she was found to have dysmorphic features suggestive of Down's syndrome, along with hypotonia, intercostal muscle retraction and a mildly distended epigastric region. She was suspected of meconium aspiration and sepsis. Her initial investigations revealed WBC of 20 100 μl, Hb of 16.8 g/dl, platelets of 114 000/μl and CRP of 10 md/l. After intravenous antibiotics, she remained stable but on Day 2 of life, she was noted to have high levels of orogastric aspirates mixed with blood. A plain X-ray revealed a dilated stomach and duodenum, with air in the distal small bowel (Fig. 1). An APT test was negative. Repeat laboratory evaluation revealed WBC of 23 200 μl, Hb of 10.1 g/dl and platelets of 140 000/μl. She was started on ranitidine 10 mg daily but she continued to have fresh blood in her orogastric tube and her hemoglobin level dropped to 8.0 g/dl with INR 10, PT 120′ and APTT 180′. She was managed accordingly and after resuscitation, an upper GI contrast study was performed to rule out malrotation or mid-gut volvulus. Her upper GI contrast suggested an incomplete duodenal obstruction (Fig. 2). To look for a source of bleeding, an upper GI endoscopy was not performed due to duodenal obstruction and a risk of perforation. The baby was taken to the operating theater for exploration to determine the cause of her ongoing hematemesis and to correct her duodenal obstruction. On exploration, her stomach and proximal duodenum were dilated with a narrowing noted in the second part of the duodenum. There was no malrotation of her gut and the rest of the bowel and solid viscera were normal. A duodenotomy of her proximal dilated duodenum revealed a complete diaphragm with a hole allowing passage of a small probe down into the distal duodenum. The mucosa of the proximal dilated duodenum was edematous and friable with multiple erosions. She underwent diamond-shaped duodenoduodenostomy for her CIDO. Her postoperative course was uneventful and hematemesis resolved. She was started on gradual nasogastric to oral feeding, which she tolerated very well. Further investigations revealed a right ectopic kidney and minor congenital cardiac defects. Her chromosomal analysis showed a karyotype of 47, XX, + 21 consistent with Down's syndrome.
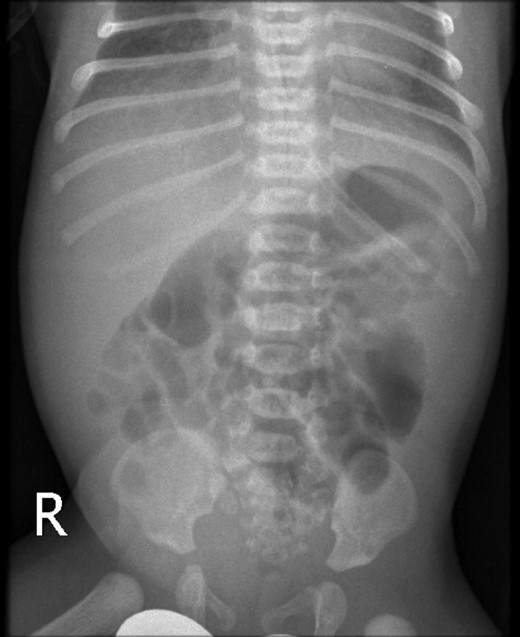
Plain X-ray abdomen on Day 3 of life showing a dilated stomach and duodenum with gas in the distal small bowel.
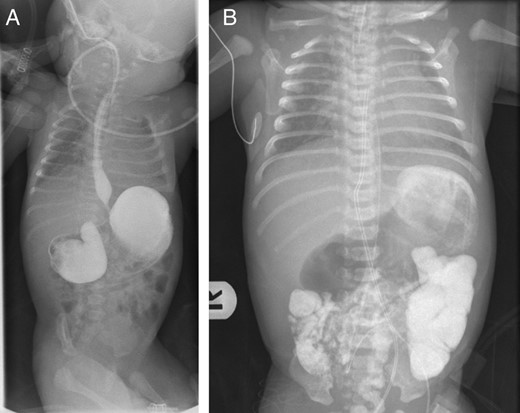
(A) Upper gastrointestinal contrast study showing a markedly distended stomach and duodenal bulb, with narrowed second part of duodenum suggesting congenital duodenal obstruction. (B) Delayed film of upper gastrointestinal contrast study showing dye passing distally suggestive of incomplete obstruction
DISCUSSION
Duodenal atresia/stenosis is a common gastrointestinal anomaly, with more than half of affected patients having associated congenital anomalies. Twenty-five to 30% of cases of duodenal atresia occur in babies with Down's syndrome [1]. Conversely, duodenal atresia is the most common gastrointestinal defect seen in children with Down's syndrome, occurring in 1–5%, with no reported association with maternal age, ethnicity or sex of the neonate [2].
Babies born with complete duodenal obstruction usually present with vomiting within the first 24–48 h of life, whereas babies with incomplete duodenal obstruction may present months later. The vomiting is usually bilious, but may be non-bilious if the lesion is preampullary, which occurs in one of five cases [1]. The presentation of incomplete duodenal obstruction with hematemesis in early life is unusual; to date, only seven such cases have been reported in the English literature [4]. Hematemesis was observed during the first few days of life in three neonates, whereas one child presented at 12 years of age. The causes of duodenal obstruction in most of these patients were internal narrowing/atresia, but obstruction in one baby was caused by extra-luminal duodenal compression from an annular pancreas (Table 1).
Description of patients with hematemesis and congenital duodenal obstruction associated with Down syndrome
| Study . | Year . | No/GA/sex . | Onset of bleeding . | Clinical features . | Site of obstruction . | Operative findings . | Associated anomalies . |
|---|---|---|---|---|---|---|---|
| Madden et al. [5] | 1956 | [4 cases] | X | Not described | Not described | Not described | Not described |
| Gilfillan et al. [6] | 1966 | 1/term/? | Day 2 | Polyhydramnios | Atresia of third part of duodenum | ? Mechanical cause of hematemesis | Not described |
| Sachs et al. [7] | 1973 | 1/?/M | 12 years | Down's syndrome | Stenosis of second part of duodenum | Duodenal ulcers due to retained foreign material | Not described |
| Bajaj et al. [8] | 1975 | 1/term/M | 1 day | Down's syndrome, Polyhydramnios | Stenosis of 2nd part of duodenum, annular pancreas | Not described | Not described |
| Chhabra et al. [4] | 1992 | 1/30 weeks/F | 1 day | Down's syndrome | First part of duodenum | Dilated duodenal bulb, incomplete rotation, isolated duodenal erosions | Congenital cardiac defect, bilateral lenticular cataracts |
| Noora et al. (current case) | 2013 | 1/term/F | 2 days | Down's syndrome | Second part of duodenum | Narrowed duodenum with web and edematous, friable duodenal mucosa proximally | Ectopic right kidney, congenital cardiac defects (minor) |
| Study . | Year . | No/GA/sex . | Onset of bleeding . | Clinical features . | Site of obstruction . | Operative findings . | Associated anomalies . |
|---|---|---|---|---|---|---|---|
| Madden et al. [5] | 1956 | [4 cases] | X | Not described | Not described | Not described | Not described |
| Gilfillan et al. [6] | 1966 | 1/term/? | Day 2 | Polyhydramnios | Atresia of third part of duodenum | ? Mechanical cause of hematemesis | Not described |
| Sachs et al. [7] | 1973 | 1/?/M | 12 years | Down's syndrome | Stenosis of second part of duodenum | Duodenal ulcers due to retained foreign material | Not described |
| Bajaj et al. [8] | 1975 | 1/term/M | 1 day | Down's syndrome, Polyhydramnios | Stenosis of 2nd part of duodenum, annular pancreas | Not described | Not described |
| Chhabra et al. [4] | 1992 | 1/30 weeks/F | 1 day | Down's syndrome | First part of duodenum | Dilated duodenal bulb, incomplete rotation, isolated duodenal erosions | Congenital cardiac defect, bilateral lenticular cataracts |
| Noora et al. (current case) | 2013 | 1/term/F | 2 days | Down's syndrome | Second part of duodenum | Narrowed duodenum with web and edematous, friable duodenal mucosa proximally | Ectopic right kidney, congenital cardiac defects (minor) |
Description of patients with hematemesis and congenital duodenal obstruction associated with Down syndrome
| Study . | Year . | No/GA/sex . | Onset of bleeding . | Clinical features . | Site of obstruction . | Operative findings . | Associated anomalies . |
|---|---|---|---|---|---|---|---|
| Madden et al. [5] | 1956 | [4 cases] | X | Not described | Not described | Not described | Not described |
| Gilfillan et al. [6] | 1966 | 1/term/? | Day 2 | Polyhydramnios | Atresia of third part of duodenum | ? Mechanical cause of hematemesis | Not described |
| Sachs et al. [7] | 1973 | 1/?/M | 12 years | Down's syndrome | Stenosis of second part of duodenum | Duodenal ulcers due to retained foreign material | Not described |
| Bajaj et al. [8] | 1975 | 1/term/M | 1 day | Down's syndrome, Polyhydramnios | Stenosis of 2nd part of duodenum, annular pancreas | Not described | Not described |
| Chhabra et al. [4] | 1992 | 1/30 weeks/F | 1 day | Down's syndrome | First part of duodenum | Dilated duodenal bulb, incomplete rotation, isolated duodenal erosions | Congenital cardiac defect, bilateral lenticular cataracts |
| Noora et al. (current case) | 2013 | 1/term/F | 2 days | Down's syndrome | Second part of duodenum | Narrowed duodenum with web and edematous, friable duodenal mucosa proximally | Ectopic right kidney, congenital cardiac defects (minor) |
| Study . | Year . | No/GA/sex . | Onset of bleeding . | Clinical features . | Site of obstruction . | Operative findings . | Associated anomalies . |
|---|---|---|---|---|---|---|---|
| Madden et al. [5] | 1956 | [4 cases] | X | Not described | Not described | Not described | Not described |
| Gilfillan et al. [6] | 1966 | 1/term/? | Day 2 | Polyhydramnios | Atresia of third part of duodenum | ? Mechanical cause of hematemesis | Not described |
| Sachs et al. [7] | 1973 | 1/?/M | 12 years | Down's syndrome | Stenosis of second part of duodenum | Duodenal ulcers due to retained foreign material | Not described |
| Bajaj et al. [8] | 1975 | 1/term/M | 1 day | Down's syndrome, Polyhydramnios | Stenosis of 2nd part of duodenum, annular pancreas | Not described | Not described |
| Chhabra et al. [4] | 1992 | 1/30 weeks/F | 1 day | Down's syndrome | First part of duodenum | Dilated duodenal bulb, incomplete rotation, isolated duodenal erosions | Congenital cardiac defect, bilateral lenticular cataracts |
| Noora et al. (current case) | 2013 | 1/term/F | 2 days | Down's syndrome | Second part of duodenum | Narrowed duodenum with web and edematous, friable duodenal mucosa proximally | Ectopic right kidney, congenital cardiac defects (minor) |
The etiology of acute bleeding in CIDO patients is not clear. It has been suggested that repeated vomiting, mechanical factors, the absence of buffering of gastric acidity and stasis of food in the dilated antrum and duodenum may contribute to hematemesis in duodenal obstruction [4–6]. In the absence of swallowed maternal blood, repeated vomiting, abnormal coagulation factors or hematemesis in our patient was likely due to duodenitis, which was noted during surgery. Duodenitis in our patient may have been caused by the stasis of gastric secretion in the duodenum due to obstruction leading to erosions; the anatomical configuration of the duodenal diaphragm, which may also have prevented the regurgitation of the neutralizing alkaline duodenal secretions and early sepsis.
The management of hematemesis secondary to gastritis/duodenitis starts by correcting hypervolemia, treatment with histamine 2 (H2) receptor blockers and fixing the underlying cause. Antacids may be dangerous to newborns, resulting in hypermagnesemia with or without hypocalcemia, antacid bezoar and intestinal perforation [4]. The hematemesis usually resolves once the primary underlying cause (duodenal obstruction) has been corrected and gastric contents can freely flow towards the duodenum, as in our patient.
The long-term risk of peptic ulceration has been assessed in children who undergo surgery for duodenal obstruction. A long-term follow-up of 169 children with duodenal atresia and stenosis found that 4 (2.4%) had peptic ulceration, with 2 of these requiring further surgical intervention [9]. These findings imply that these patients may need follow-up throughout childhood and adolescence.
In summary, congenital duodenal obstruction carries a risk of duodenitis in newborns, and they may present with acute hematemesis. The management includes early surgery to relieve the obstruction.
CONFLICT OF INTEREST STATEMENT
The authors declare that there are no conflicts of interest.
ACKNOWLEDGEMENTS
We gratefully acknowledge the Medical Research Centre, Hamad Medical Corporation, Doha, Qatar, for their support in publishing this article.



