-
PDF
- Split View
-
Views
-
Cite
Cite
William Maclean, Karoly Szentpáli, Large gallstone impaction at a Meckel's diverticulum causing perforation and localized peritonitis: report of a case, Journal of Surgical Case Reports, Volume 2013, Issue 12, December 2013, rjt097, https://doi.org/10.1093/jscr/rjt097
Close - Share Icon Share
Abstract
We are reporting a successful laparoscopic resection of a perforated Meckel's Diverticulum (MD) causing localized peritonitis due to an impacted gallstone. MD is a small benign pouch on the wall of the small intestine that is present in ∼2% of the population. It results from a failure of complete obliteration of the omphalomesenteric duct. MD is mainly lined by ileal mucosa; however, other ectopic tissue types can be found including gastric, duodenal, colonic, pancreatic, Brunner's glands, hepatobiliary tissue and endometrial mucosa. Most reported complications include bleeding, infection and obstruction. With relevance to this report, we can find no more than two reports of a large gallstone impacting the neck of the MD and causing ileus, and we were unable to find any reports that mention perforation due to impaction at the neck of an MD.
INTRODUCTION
We are reporting a successful laparoscopic resection of a perforated Meckel's Diverticulum (MD) causing localized peritonitis due to an impacted gallstone.
MD is a small benign pouch on the wall of the small intestine that is present in ∼2% of the population [1]. It results from a failure of complete obliteration of the omphalomesenteric duct [2]. MD is mainly lined by ileal mucosa; however, other ectopic tissue types can be found, including gastric, duodenal, colonic, pancreatic, Brunner's glands, hepatobiliary tissue and endometrial mucosa [3]. Most reported complications include bleeding, infection and obstruction. With relevance to this report, we can find no more than two reports of a large gallstone impacting the neck of the MD and causing ileus [4, 5], and we were unable to find any reports that mention perforation due to impaction at the neck of an MD.
CASE REPORT
An 82-year-old man was admitted to the hospital with a 12-h history of right iliac fossa pain. He woke up with the pain, which gradually progressed throughout the course of the day. He felt feverish with anorexia and nausea; there were no other bowel symptoms. On admission, physical examination revealed a soft abdomen with maximal tenderness over Mcburney's point, localized percussion tenderness and Rovsing's test was positive.
He had low-grade pyrexia and his inflammatory markers were raised with a white cell count of 15.2 × 109/l and a C-reactive protein of 62. Plain chest and abdominal radiographs were unremarkable. Past medical history included gastroplasty and multiple dilatations for a benign oesophageal stricture, he was otherwise well.
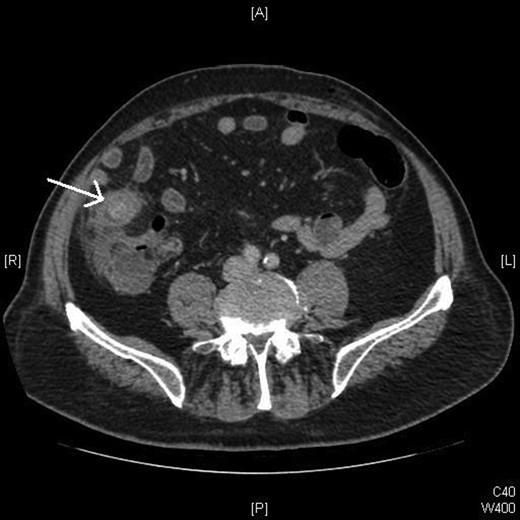
A computed tomography (CT) scan was performed in light of the patient's age (Fig. 1), which reported ‘a dilated fluid filled appendix, containing an appendicolith.’ Laparoscopic appendicectomy was therefore planned (Fig. 1).
During laparoscopy, there was evidence of localized peritonitis, and an inflamed MD was found containing a large gallstone that had eroded through the wall. The appendix appeared to be normal (Fig. 2).

Intraoperative picture demonstrating the gallstone entrapped in the MD.
The operation remained laparoscopic and the MD was resected using an Endo GIA™ 45 stapler, allowing continuity of the small bowel. The specimen and gallstone were extracted through the superior umbilical port site in an endobag.
The specimen was extracted and confirmed a 3×2.5 cm gallstone based on its yellow-green colour and laminated crystalline appearance [6] (Fig. 3).

Our patient recovered well postoperatively and was discharged 2 days later. At a 3-week outpatient follow-up, the patient was back to his usual diet and feeling well. The histology report confirmed that the specimen was an MD with gangrenous inflammation, focal perforation and no evidence of malignancy.
DISCUSSION
Pathology relating to Meckel's diverticula still causes diagnostic dilemma in cases of right iliac fossa pain. In the available literature, MD-related complications are bleeding, inflammatory changes and rarely obstruction. We therefore believe this to be the first reported case of perforation of an MD due to a gallstone, which was treated with a minimally invasive surgical procedure.
Despite the rarity of this case, it demonstrates the importance of the differential diagnosis for right iliac fossa pain. Laparoscopy is an excellent diagnostic and therapeutic tool, which is coupled with advancing equipment and techniques; this has enabled adaptability and diversity in procedures that can now be performed. In this case, a swift diagnosis of the perforated MD was achieved, and it was resected effectively and safely along with the gallstone without the need for converting to an open procedure.
Although the CT scan was misleading on this occasion, we would still strongly advocate its use in the elderly patients prior to diagnostic laparoscopy. As a result of CT, we were able to rule out other causes of right iliac fossa pain such as diverticulitis or a tumour that may not have warranted immediate surgery.



