-
PDF
- Split View
-
Views
-
Cite
Cite
Nicholas G. Matthees, James A. Mankin, Olga M. Kalinkin, Randy R. Richardson, A rare opportunity for conservative treatment in a case of blunt trauma to the supradiaphragmatic inferior vena cava, Journal of Surgical Case Reports, Volume 2013, Issue 11, November 2013, rjt092, https://doi.org/10.1093/jscr/rjt092
Close - Share Icon Share
Abstract
Injuries to the inferior vena cava (IVC) secondary to blunt trauma are rare and occur in only 1–10% of all blunt trauma patients. Management of these injuries has not been subjected to major studies, but several case reports and small retrospective studies have demonstrated that management can be tailored to the hemodynamic status of the patient; this is similar to the management of blunt liver injuries. Stable patients whose injuries have achieved local venous tamponade have been successfully treated without surgical intervention, while unstable patients require operative management. Regardless of patient status, however, IVC injuries are highly fatal with mortality rates between 70 and 90%. This report describes the case of a patient with a blunt traumatic injury to the supradiaphragmatic IVC with development of a pseudoaneurysm who was successfully managed conservatively.
INTRODUCTION
Blunt injury to the inferior vena cava (IVC) is rare, occurring in only 1–10% of blunt trauma patients [1]. Deceleration causes shear forces on vessels, including the atriocaval junction and the hepatic veins, and can quickly produce rapid, uncontrollable hemorrhage. The liver is second to the spleen as the most commonly injured abdominal organ. Historically, blunt liver injuries have been managed according to the patient's hemodynamic status [2]. A case of an IVC pseudoaneurysm (contained traumatic supradiaphragmatic rupture of the IVC and associated pericaval hematoma) without involvement of the pericardium is reported, which required no surgical intervention.
CASE REPORT
A 20-year-old female was the restrained driver of a vehicle traveling ∼45 miles per hour when her vehicle crashed into a city bus. She was extricated on scene by emergency responders and brought to the trauma bay alert, oriented and in stable condition complaining of pain on deep inspiration as well as left leg pain. She denied any abdominal pain or light-headedness. Vital signs on arrival were heart rate of 115 bpm, respiratory rate of 20 breaths per minute and blood pressure of 101/76 mmHg; her Glasgow coma scale was 15. The initial chest radiograph showed a small, right-sided pneumothorax and pulmonary contusions. Two radiographic views of the left leg revealed comminuted, mildly displaced tibia and fibula fractures. Computed tomography (CT) scans of the brain and neck were unremarkable. A contrast-enhanced chest CT scan demonstrated non-displaced right lateral second and third rib fractures, right upper lobe pulmonary contusions with laceration and a small pneumothorax, partially visualized grade 5 liver laceration with active contrast extravasation, and an acute, traumatic supradiaphragmatic IVC injury with an associated moderate hematoma and contrast extravasation that appeared to be contained, as seen in Figs 1 and 2. In view of incompletely imaged critical findings of the upper abdomen and continued hemodynamic stability of the patient, a dedicated abdomen and pelvis CT scan, seen in Figs 3–5, was performed 20 min later, which showed a stable 1.3 cm pseudoaneurysm of the supradiaphragmatic IVC without extension into the pericardium, stable moderate pericaval hematoma surrounding the injury, stable grade 5 liver laceration and a trace amount of fluid in the peritoneal cavity. A liver transplant surgeon and a cardiovascular surgeon were consulted due to the presence of acute traumatic suprahepatic IVC pseudoaneurysm.
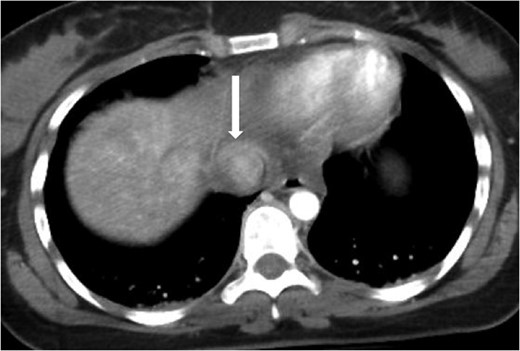
Axial contrast-enhanced CT of the chest showing abnormal contour of the supradiaphragmatic IVC with ventrally and laterally confined contrast extravasation (arrow) consistent with a pseudoaneurysm surrounded by pericaval hematoma.

Coronal contrast-enhanced CT of the chest showing abnormal contour of the supradiaphragmatic IVC with ventrally and laterally confined contrast extravasation (arrow) consistent with a pseudoaneurysm surrounded by pericaval hematoma as well as a segment 8 hepatic hypodensity consistent with liver laceration and focal area of contrast extravasation (arrowhead).
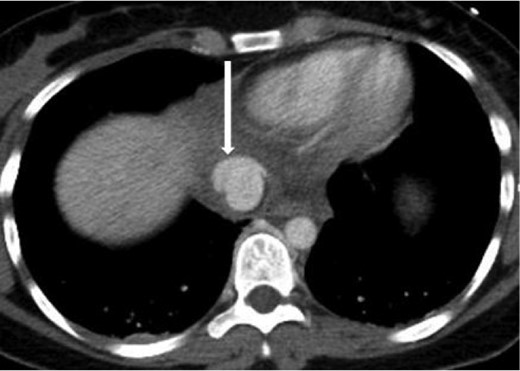
Axial contrast-enhanced CT of the abdomen performed 30 min after the initial CT of the chest showing persistence of the abnormal contour of the supradiaphragmatic IVC with contrast extravasation confined laterally and ventrally (arrow), nonexpanding pericaval hematoma.

Coronal contrast-enhanced CT of the abdomen performed 30 min after the initial CT of the chest showing persistence of the abnormal contour of the supradiaphragmatic IVC with contrast extravasation confined laterally and ventrally (arrow), nonexpanding pericaval hematoma and a segment 8 hypodensity (arrowhead) consistent with liver laceration.

Sagittal contrast-enhanced CT of the abdomen performed 30 min after the initial CT of the chest showing persistence of the abnormal contour of the supradiaphragmatic IVC with contrast extravasation confined laterally and ventrally (arrow), nonexpanding pericaval hematoma.
The patient remained in stable hemodynamic condition over the subsequent 3 h, and the decision was made to obtain an IVC venogram, depicted in Fig. 6, which showed a small focal contour irregularity of the suprahepatic IVC and slight irregularity of the right middle vein consistent with a pseudoaneurysm and no active contrast extravasation. Conservative management of the hepatic laceration and IVC injury was continued in the intensive care unit with strict bed rest. On post trauma day 3, her tibia and fibula fractures were repaired without complications. The patient was discharged on post trauma day 7.

Inferior venacavagram showing a mild contour irregularity of the suprahepatic IVC without contrast extravasation (arrow) and a slight contour irregularity of the middle hepatic vein without contrast extravasation (arrowhead) consistent with a pseudoaneurysm of the IVC and right middle hepatic vein.
DISCUSSION
Injuries to the IVC are relatively uncommon in the setting of blunt abdominal trauma and are rarely isolated. These injuries are usually lethal even before arriving to the hospital [3]. In one study of 10 patients who presented with IVC injury secondary to blunt trauma, there was a 70% mortality rate [4]. Depending on the location of injury, death is due to exsanguination or cardiac tamponade. Typically, trauma to the IVC is associated with liver injury and the liver is the second most commonly injured abdominal organ in blunt trauma. Damage to juxtahepatic veins constitutes a small proportion of all liver injuries, but the mortality rate is between 50 and 80% with most deaths caused by exsanguination [5]. In current literature, there are few studies that scrutinize the repair of injuries to the vena cava and juxtahepatic veins, as these injuries are rare and usually fatal before treatment can be initiated.
Treatment of IVC injuries can include but is not limited to definitive vascular repair, damage control procedures (ligation, shunting or packing) or a conservative approach. Decision to repair an IVC injury is based on the location, extent of injury and on the hemodynamic status of the patient. Patients who are stable or whose caval injuries have reached spontaneous vascular tamponade, typically through containment by the liver capsule, diaphragm or suspensory ligaments, have been successfully managed with conservative treatment [5]. Operative strategies have been employed for unstable patients, patients with large defects of the IVC and for patients whose caval hematomas are not contained [4–7]. The suprahepatic region of the IVC is challenging for surgical intervention, as it requires dividing the falciform ligament, cross clamping, mobilizing the damaged IVC segment and extending the abdominal incision into a full sternotomy. Intervention is associated with high perioperative mortality and morbidity rates and long-term complications, including IVC stenosis and thrombosis [8–10]. Nearly, all case reports describing the repair of these lesions involve the use of cardio-pulmonary bypass and grafting the damaged vessels and have a high mortality rate between 70 and 90% [1, 3–5]. There is one recent report, however, which described the successful reconstruction of an extrapericardial rupture of the IVC using a cross-clamping technique and a Gore-Tex prosthesis [6]. In light of the clinical and hemodynamic stability of our patient, imaging findings of a contained suprahepatic IVC pseudoaneurysm, challenging operative region for intervention and risk of morbidity associated with operative treatment, the decision was made for conservative management.
ACKNOWLEDGEMENTS
The authors thank Dr. Jeffrey Brink and Dr. Kenneth Ashton for their assistance in the management of our patient. The authors received no funding for this case and have no financial disclosures to report.



