-
PDF
- Split View
-
Views
-
Cite
Cite
Elroy Patrick Weledji, George Enow Orock, Leopold Aminde, Massive prolapsed haemorrhoids managed by ablation and correction in a poor resourced area, Journal of Surgical Case Reports, Volume 2013, Issue 11, November 2013, rjt094, https://doi.org/10.1093/jscr/rjt094
Close - Share Icon Share
Abstract
More recently some patients with rectal mucosal prolapse and obstructive defaecation have been treated with the procedure for prolapse and haemorrhoids. We report a case of symptomatic chronic circumferentially prolapsed haemorrhoids that had several failed attempts at surgical repair. This was finally managed by ablation and correction of the associated rectal mucosal prolapse by a modified ‘Delorme's procedure akin to a stapled anopexy.
INTRODUCTION
Haemorrhoidal disease is common [1]. When the supporting submucosal fibres fragment due to prolonged straining during defaecation of hard stools, the anal cushions are no longer restrained from engorging excessively with blood and this results in bleeding and prolapse [1, 2]. Thus, prolapsed haemorrhoids may be associated with rectal prolapse. After other life-threatening diseases have been excluded, in the past, severe circumferential prolapse with massive engorgement of both external and internal haemorrhoidal plexuses required extensive ablation to ensure adequate treatment with subsequent mucocutaneous reconstitution [2]. This may unfortunately ignore an associated rectal prolapse [3–6].
CASE REPORT
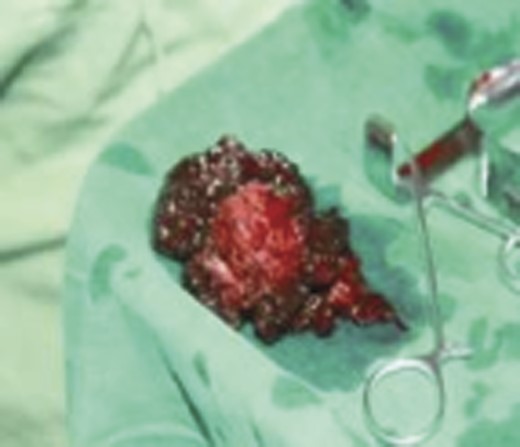
A 75-year-old man was admitted electively to the hospital for assessment and management of persistent prolapsed haemorrhoids (Fig. 1), despite recurrent surgery, thrice in the past 3 years. This was associated with constipation and straining at stool. There was fresh rectal bleeding not mixed with stool during defaecation. He had no loss of appetite nor weight loss. On examination, he was pale and tired-looking. Chest, cardiovascular and abdominal examinations were unremarkable. A rectal examination revealed massive, irreducible, prolapsed, circumferential haemorrhoids that were ulcerating, bleeding and occluding the anal orifice. The external components showed squamous hyperplasia with keratinization and a frond-like, friable appearance. Proctoscopy revealed solid palpable internal haemorhoidal components with a similar pigmentation (acanthosis) as the external components at their classic anatomical positions—the left lateral, right posterior and right anterior positions—but no definite rectal mucosal lesion was seen. Rigid sigmoidoscopy was normal. He was found to be anaemic with a haemoglobin level of 7 gm/dl. The differential diagnosis included an extensive locally advanced anal carcinoma, an extensive fungating perianal condylomata acuminata (Buschke-Lowenstein's disease), chronically prolapsed (fourth degree) haemorrhoids with external components or a chronic rectal prolapse. A biopsy revealed haematoma consistent with a haemorrhoid. His iron-deficiency anaemia was corrected by blood transfusion prior to an examination under anaesthesia.

Prolapsed thrombosed fourth degree haemorrhoids (with permission).
In the lithotomy position, an extensive Milligan–Morgan haemorrhoidectomy with mucocutaneus skin bridges and high ligation was performed (Fig. 2). The external component of the haemorrhoidal tissue disintegrated into black clots on dissection (Fig. 3). An intussucepting rectal prolapse with a sulcus between the prolapse and the edge of the anal canal became evident. A modified Delorme's procedure was done by excising the redundant mucosal sleeve, reducing the prolapse and plicating the prolapsed muscle wall to the proximal rectal mucosa cuff (Fig. 2). However, as most of the anal canal skin at the level of the dentate line was incorporated in the extensive internal and external haemorrhoidal engorgement and thus been excised en-bloc, the distal component of the plication was sutured but to the fascia (epimysium) overlying the internal anal sphincter. Pouting of the rectal mucosa at the anal orifice causing a mucoid leak was prevented by not stitching to the perianal skin. The wide perianal skin defects were approximated to facilitate healing and reduce pain (Fig. 4). The estimated intra-operative blood loss was <300 ml. The anal sphincteric tone was satisfactory. His postoperative haemoglobin level was 9 g/l, for which he received a further unit of blood. A laxative (lactulose) was prescribed and the patient mobilized. He made good recovery with no passive or active (urge) incontinence. He was discharged on the eighth postoperative day on iron supplements and advised a high-fibre diet and regular follow-up.


Post Milligan–Morgan haemorrhoidectomy and modified Delorme's correction (with permission).
DISCUSSION
This case illustrates the importance of excluding an underlying rectal prolapse in a patient with recurrent haemorrhoids despite conventional haemorrhoidectomy. The introduction of less invasive surgical modalities, which offer good symptomatic control and less postoperative pain, has reduced the number of patients requiring conventional haemorrhoidectomy [3]. Conventional haemorrhoidectomy deals with the symptoms alone without due regard to restoration of the normal physiology by fixation of the congested anal cushions. On the other hand, stapled haemorhoidopexy tries to correct the primary pathology, by after reducing the prolapsed haemorrhoidal tissue, the redundant lower rectal mucosa is excised and the prolapse fixed back into its proper place on the wall of the anal canal [4, 5]. The fixation into muscle helps prevent subsequent re-dislodgement and recurrence. There is less postoperative pain as the procedure avoids the sensitive anoderm below the dentate line, which is usually incorporated in conventional haemorrhoidectomy [6]. In this case, the true nature of the rectal prolapse was not diagnosed till the Milligan–Morgan procedure was completed. In the situation with massive prolapsed haemorrhoids >3–4 cm outside the anal verge, there is not enough space with the staple housing to contain it, and thus a circular PPH (proximate –Ethicon) stapler may be found to be effective [7]. In this patient with such a wide extension of the external component outside the anal verge, a more expensive alternative might be to use two staplers simultaneously [8]. In areas with limited health resources, an alternative surgical method for the irreducible massive circumferential prolapsed (fourth degree) haemorrhoids is an excision followed by a modified ‘Delorme's’ correction approach, if there is associated rectal prolapse as in this case, so as to reduce rectal mobility and prevent recurrence [9, 10].
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.



