-
PDF
- Split View
-
Views
-
Cite
Cite
T.I. Arthur, C.J. Gillespie, W. Butcher, C.T. Lu, Pseudoaneurysm of the internal iliac artery resulting in massive per-rectal bleeding, Journal of Surgical Case Reports, Volume 2013, Issue 10, October 2013, rjt069, https://doi.org/10.1093/jscr/rjt069
Close - Share Icon Share
Abstract
Rectal bleeding is a common reason for presentation to hospital, with large bleeds most commonly caused by diverticular disease and angiodysplasia. Here we present an unusual aetiology of massive per-rectal bleeding attributable to pseudoaneurysm of the internal iliac artery leading to an arterial fistula to the distal large bowel. It is hoped the case will serve as a reminder that rectal bleeding can have a less common aetiology.
INTRODUCTION
The terms pseudoaneurysm, false aneurysm and pulsating haematoma all describe the same phenomenon, that is a defect in the vascular wall leading to an extra-vascular haematoma that freely communicates with the intravascular space [1]. Once in its fully developed state, it may have a cavity with an endothelial lining in continuity with that of the artery [2]. Isolated internal iliac aneurysms are an uncommon entity and isolated pseudoaneurysms of the internal iliac artery even more so. Here we present an unusual aetiology of massive per-rectal bleeding attributable to pseudoaneurysm of the internal iliac artery, leading to arterio-colic fistula.
CASE REPORT
An 83-year-old male presented to the emergency department with a history of passing a cupful of bright red blood with his morning bowel motion. His past medical history was significant for diverticular disease, which had resulted in a perforated sigmoid colon 23 years before, requiring Hartmann's procedure which was subsequently reversed.
He arrived with a blood pressure of 130/75 mmHg and a tachycardia of 104 beats per minute. The haemoglobin level was 13.7 g/l on arrival. Rigid sigmoidoscopy in the emergency department revealed an empty rectum with copious amounts of stool and blood up to 10 cm. The patient was presumptively diagnosed with a diverticular bleed and admitted to the general surgical unit for observation. The following day a further significant per-rectal bleed occurred on the ward, associated with chest pain and ECG changes. Blood tests revealed a haemoglobin drop to 11.3 g/l and an elevated serum troponin level of 0.19 μg/l. Myocardial infarction was diagnosed and he was placed on telemetry in a cardiac monitoring unit. A further massive per-rectal bleed was reported on the ward that evening, with a subsequent drop in haemoglobin to 7.7 g/l. Resuscitation was commenced with three units of packed red blood cells and a mesenteric CT angiogram arranged.
An arterial phase CT abdomen with IV contrast was performed. This revealed a contrast blush within the descending colon closely associated with an aneurysm of the internal iliac artery. The possibility of an arterial fistula to the colon was raised, and a vascular surgery consult was sought. Angiography confirmed a false aneurysm arising from the proximal aspect of the left internal iliac artery along its medial and inferior wall. Endovascular coil embolization was performed with occlusion of the vessel at the level of the aneurysm.
No further episodes of per-rectal bleeding have been reported in 3 months following embolization. Follow-up colonoscopy revealed multiple diverticulae in the descending colon, but the site of the previous bleed was not evident.
DISCUSSION
This patient had an isolated pseudoaneurysm of the internal iliac artery resulting in an arterio-colic fistula (Fig. 1). Isolated aneurysms of the internal iliac artery themselves are a rare phenomenon, estimated to account for only 0.3–0.4% of all intra-abdominal aneurysms. Forty per cent of patients with isolated internal iliac aneurysms will present with a rupture, with mortality estimated to exceed 50% in such patient groups [3].
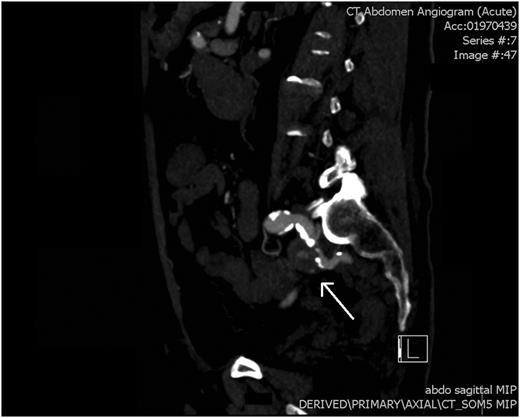
CT angiogram: a saggital view showing pseudoaneurysm of the left internal iliac artery (white arrow).
Pseudoaneurysms are usually secondary to trauma, but may be iatrogenic following intravascular catheterization. They have also been reported as a rare complication of pelvic surgery [4]. Over the last few decades there has been an increase in the incidence of pseudoaneurysms in general, due to an increase in interventional vascular access [5]. Infections, connective tissue disorders, vasculitis and erosion secondary to malignancy may also be implicated in the formation of pseudoaneurysms [6].
In a review of the literature on isolated internal iliac aneurysms, Dix et al. [7] found ∼6% of patients with such aneurysms will present with rectal bleeding. Cases described have included iliac-rectal fistula following coil occlusion of an iliac aneurysm and fistulous connection between aneurysm and caecal carcinoma [8].
The aetiology of this patient's pseudoaneurysm is unclear. Diverticulitis in and of itself is not known as a cause for pseudoaneurysm formation; however, pelvic infections have been implicated. This patient had an episode of diverticular disease 23 years previously which required a Hartman's procedure, this was reversed 6months later. Whether the cause of the pseudoaneurysm was mycotic or traumatic (secondary to either the first or second stage procedure) is a matter of conjecture. Anastamotic leak post-colostomy reversal could have been implicated, however, on imaging the pseudoaneurysm communicates with a large bowel ∼5 cm proximal to the anastamotic suture line.
Regardless of the aetiology, if the pseudoaneurysm occurred around the time of his original operation, it remained quiescent for 23 years before causing symptoms. The reported mortality rate for ruptured internal iliac aneurysms is ∼50%—fortunately in this case the diagnosis was made rapidly with imaging and immediate treatment led to a good outcome. The efficacy of expedient angiography in per-rectal bleeding has been shown previously, with mesenteric embolization clinically successful in 76% of cases of lower gastrointestinal bleeding with active bleeding on angiography [9]. Aggressive management of internal iliac aneurysms, regardless of the mode of presentation, is required to avoid the high morbidity and mortality associated with rupture. They can be managed with open or endovascular techniques, with a tendency towards the latter over the previous years. Occlusion of the internal iliac artery can result in multiple sequelae, including lumbosacral plexus ischaemia, buttock necrosis, colorectal infarction, impotence and buttock claudication. Buttock claudication, the most common of these complications, is estimated to occur in 28–40% of patients, with severe debilitating claudication in 9% [10]. At follow-up, no symptomology suggestive of claudication was elicited in our patient.
Per-rectal bleeding is a common presentation with most cases of massive bleeding caused by diverticular disease and angiodysplasia. The above case will hopefully serve as a reminder that per-rectal bleeding can have a less common aetiology. Identification of an iliac aneurysm on imaging for rectal bleeding should alert the clinician to the possibility of an arterial fistula to the colon.



