-
PDF
- Split View
-
Views
-
Cite
Cite
Akhil A. Tawari, Vishal D. Bahuva, Arvind B. Goregaonkar, Subaraman R., A rare case of open anterior hip dislocation, Journal of Surgical Case Reports, Volume 2013, Issue 1, January 2013, rjs035, https://doi.org/10.1093/jscr/rjs035
Close - Share Icon Share
Abstract
Anterior hip dislocation is much less frequent when compared with posterior dislocation of the hip joint, with open dislocation being still rarer. We report a case of an open anterior hip dislocation in a 23-year-old male who presented to us in the emergency department, and also present a review of the literature.
INTRODUCTION
The incidence of patients with traumatic dislocations due to high velocity trauma is constantly increasing. While the majority of them are posterior dislocations, anterior dislocations comprise less than 10–15% [1] of all dislocations. An open anterior dislocation results in serious management problems. One has to deal with higher chances of infection on one hand, and higher complication rates, such as avascular necrosis, on the other hand. Such problems and complications are more common in anterior than posterior dislocations.
CASE REPORT
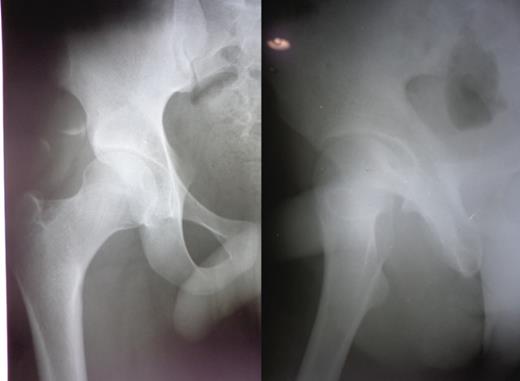
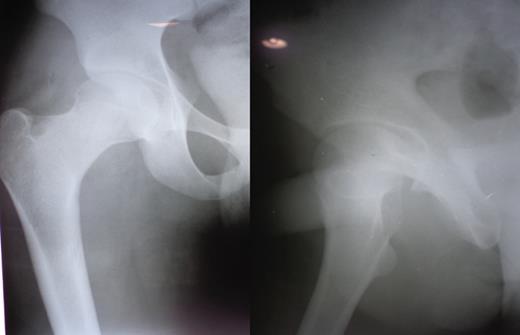
A 23-year-old male pavement dweller was brought to the emergency department of this hospital after being hit by a tempo. The patient was in a state of shock with an open right-sided anterior hip dislocation with the femoral head being visible in the inguinal region (Fig. 1). The neurovascular status of the right lower limb was intact. Immediate resuscitation was done and hip radiographs (Fig. 1) were taken, which showed an anterior-inferior dislocation with an inferior pubic ramus fracture on the left side. The patient was immediately transferred to the operating room where the wound was thoroughly debrided and the femoral head was relocated within 5 hours of sustaining the trauma (Fig. 2). The wound after surgical debridement was 8 × 6 cm in dimensions, which was primarily closed after checking for the stability of the reduction. The patient was started on intravenous metronidazole, amikacin and ceftriaxone for 5 days, followed by oral amoxicillin for a week. The patient was kept non-weight-bearing on skin traction for 6 weeks. The wound healed satisfactorily with no evidence of infection, nor any episode of re-dislocation at 6 months (Fig. 3). The patient was unfortunately lost to follow-up.
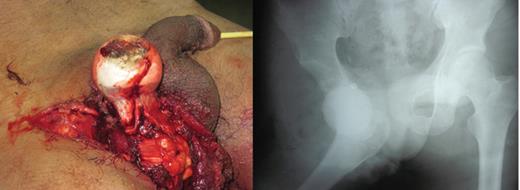
Figure and radiograph showing an open anterior hip dislocation.
DISCUSSION
Traumatic hip dislocations are serious injuries because the hip joint is extremely stable and considerable force is necessary to produce its dislocation. Open hip dislocation remains a rare occurrence due to the bulky muscle envelope surrounding the deeply situated hip joint. Traumatic hip dislocations occur in the third decade of life in ∼35% of the cases with 75% of the injuries occurring in males [1]. The posterior dislocation of the hip is by far the most common type with a reported ratio of anterior to posterior dislocations ranging from 1:10 to 1:19 [2, 3]. Anterior hip dislocation occurs when the knee strikes a dashboard with the thigh abducted or due to fall from a considerable height or from a blow to the back while in a squatting position [2, 3]. The neck of the femur or the greater trochanter impinges on the rim of the acetabulum and thereby levers the head of the femur out of the acetabulum through a tear in the anterior hip capsule. Anterior dislocations are of two main types depending upon the amount of hip flexion at the time of impact: superior, where the femoral head is displaced into the iliac or pubic region and inferior, where the femoral head lies in the obturator region. Anterior hip dislocations can be associated with femoral neurovascular injury [4], femoral head fractures [5] and acetabular fractures. The initial treatment for a patient with hip dislocation is gentle and prompt reduction within 6 hours and preferably under general anaesthesia to prevent and minimize complications. An important complication following traumatic dislocation of the hip is prolonged and irreversible ischaemia of the head of the femur leading to osteonecrosis in 10–30% or more of cases, particularly if the dislocation is accompanied by severe bone destruction. The objective of treatment is to obtain an anatomical reduction with congruous hip joint surfaces. Instability, loose fragment retention in the hip joint or incomplete reduction, severe soft-tissue injury, irreversible damage to femoral head vascularity and infection preclude a good result.
In our case, the most plausible explanation for the mechanism of injury seems to be forceful external rotation, abduction and hip hyperextension. This resulted in tearing of the medial capsulo-ligamentous structure followed by tearing of muscles and ultimately the skin in the region of the groin. Thorough debridement and timely reduction resulted in a good outcome at 6 months with no evidence of infection or re-dislocation. Unfortunately the patient was lost to follow-up. Review of the literature reveals only three previous reported cases of open anterior hip dislocation in adults [6–8]. Two are anterior–superior dislocations [6, 8] and only one case of anterior-inferior dislocation [7]. In all of them immediate reduction and adequate debridement with antibiotic coverage was carried out and the patients had an uneventful recovery. Thus, there are certain factors that are under the control of surgeons, such as the promptness and adequacy of reduction and thorough debridement, which, if done properly, can provide good results.



