-
PDF
- Split View
-
Views
-
Cite
Cite
X Zhang, A Shah, SC Ward, Mucinous cystic neoplasm of the liver: mimicker of echinococcal cyst, Journal of Surgical Case Reports, Volume 2012, Issue 9, September 2012, Page 5, https://doi.org/10.1093/jscr/2012.9.5
Close - Share Icon Share
Abstract
Mucinous cystic neoplasm of the liver (MCN) is uncommon and sometimes misdiagnosed as Echinococcal cyst, especially when patient with history of echinococcus infection. We report an asymptomatic 60 year-old woman with history of echinococcal cyst in the liver which was resected approximately 20 years ago, developed a new liver cystic lesion approximately 7 years after resection. Contrast enhanced computed tomography demonstrated a 7.4 x 5.6 x 5.4 cm cystic lesion in the right hepatic lobe with thin septations and no enhancing solid components. Though the serum antibody to Echinococcus was negative, the diagnosis of Echinococcal cyst was made and the patient was started empirically on Echinococcal therapy based on her clinical history and imaging findings. Post treatment CT scan showed that the cyst continued to grow. A partial right lobectomy was performed and the final diagnosis was mucinous cystic neoplasm of the liver (MCN).
INTRODUCTION
Mucinous cystic neoplasm of the liver (MCN) is uncommon and sometimes misdiagnosed as Echinococcal cyst, especially when patient with history of echinococcus infection.
CASE REPORT
An asymptomatic 60 year-old woman with history of hypertension, diabetes mellitus, arthritis, and echinococcal cyst in the liver which was resected approximately 20 years ago, developed a new liver cystic lesion approximately 7 years after resection. The lesion appeared to slowly increase in size on follow up imaging studies. The patient remained asymptomatic. Contrast enhanced computed tomography (CT) demonstrated a 7.4 x 5.6 x 5.4 cm cystic lesion in the right hepatic lobe with thin septations and no enhancing solid components. Though the serum antibody to Echinococcus was negative, the diagnosis of Echinococcal cyst was made and the patient was started empirically on Echinococcal therapy with Albendazole 400mg daily for 2 months based on her clinical history and imaging findings. Post treatment CT scan showed that the cyst continued to grow (10.5 x 9.1 x 8.2 cm) (Fig. 1A). A partial right lobectomy was performed. Pathologic examination of the 755g resection specimen revealed an 8 x 7 x 5 cm subcapsular multiloculated cyst. The cystic structures ranged from 0.4 cm to 7.2 cm in greatest dimension (Fig. 1B). The cyst contained clear yellow fluid with a smooth inner cyst wall. The uninvolved hepatic parenchyma was grossly unremarkable. Histopathologically, the cysts were lined by mucinous columnar and/or cuboidal epithelium with surrounding subepithelial ovarian-type stroma (Fig. 1C). The ovarian-type stroma was positive for oestrogen receptor (ER) (Fig. 1D), progesterone receptor (PR), and inhibin; while the lining epithelial cells were positive for epithelial membrane antigen (EMA), carcinoembryonic antigen (CEA), and mucicarmine. These are typical features for pathologic diagnosis of mucinous cystic neoplasm of the liver (MCN).
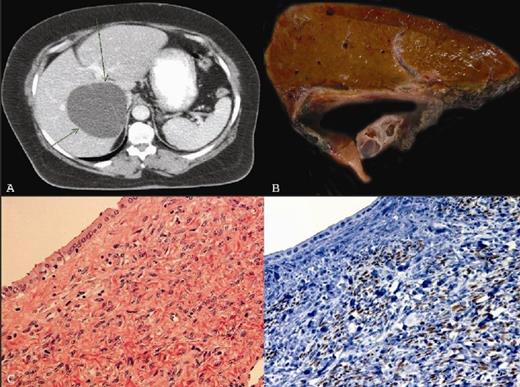
1A) Contrast enhanced computed tomography (CT) demonstrating a cystic lesion in the right hepatic lobe with thin septations. 1B) Partial right lobectomy specimen showing subcapsular multiloculated cyst. 1C) The multiloculated cysts lined by mucinous columnar and/or cuboidal epithelium with surrounding subepithelial ovarian-type stroma (H&E, X 400). 1D) The ovarian-type stroma was positive for oestrogen receptor (Immunohistochemistry, X400)
DISCUSSION
MCNs, previously called hepatobiliary cystadenoma, are rare, and are seen almost exclusively in women (age from 21 to 67 years with mean age of 45 years) with only a few cases reported in men and children(1,2). The origin of MCNs is still unclear. MCNs may develop from endodermal immature stroma or primary yolk sac cells implanted during embryogenesis. The expression of ER/PR/inhibin in the ovarian-type stroma also supports a putative role for female hormones in the tumorigenesis. The differential diagnosis includes simple cysts, echinococcal cysts, liver abscesses, cystic degeneration of a liver neoplasm, Caroli’s disease, posttraumatic cysts, and polycystic diseases. Several reports have shown that MCNs were interpreted as echinococcal cyst (3). Clinical echinococcosis history and positive serologic test may help the diagnosis of echinococcal cyst. However, the sensitivity of serodiagnostic tests for echinococcosis is only 80% to 90%. MCNs can progress to invasive carcinoma over a period of many years. When present, an associated invasive carcinoma is usually limited to the primary neoplasm, and complete surgical resection is often feasible. However, invasive carcinoma can invade to liver parenchyma, or metastasize. The prognosis for patients with a noninvasive MCN is excellent with complete resection. Carcinomas arising in association with MCNs have a better prognosis than that of cholangiocarcinoma.



