-
PDF
- Split View
-
Views
-
Cite
Cite
S Singh, A Batra, AK Sangwaiya, N Marwah, KN Rattan, R Sen, Heterotopic pancreas presenting as ileoileal intussusception, Journal of Surgical Case Reports, Volume 2012, Issue 9, September 2012, Page 13, https://doi.org/10.1093/jscr/2012.9.13
Close - Share Icon Share
Abstract
Heterotopic, aberrant or ectopic pancreas is defined as the presence of pancreatic tissue in topographic anomaly, with no anatomical, neural or vascular connection to the normal pancreas. It is a rare condition found mainly in stomach, duodenum and jejunum. Ileal heterotopic pancreas is an uncommon condition and has been rarely reported in children so far. Hereby we report a case of heterotopic pancreas presenting as ileal poyp leading to ileoileal intussusception in a 12 year child.
INTRODUCTION
Pancreatic heterotopia is defined as the presence, outside its usual location, of pancreatic tissue which lacks anatomical and vascular continuity with the pancreas proper (1). The heterotopic pancreas (HP) is a relatively uncommon congenital anomaly, with an incidence between 0.55% and 13.7% in autopsy series and mean frequency between 1 and 2%. HP has been found in all age groups, predominantly in the sixth decade of life (2). It has rarely been reported in pediatric cases. The usual locations of HP are in the stomach in 25-38% cases, the duodenum in 17-36% and the jejunum in 15-22% of cases. It is usually silent but it may become clinically evident when complicated by inflammation, bleeding, obstruction or malignant transformation (3). Symptomatic patients require surgical exploration in order to obtain a definitive diagnosis and to exclude malignancy. Local excision is adequate if the lesion looks benign (4).
CASE REPORT
A 12 years old male child presented with severe abdominal pain and intermittent vomiting, not relieved with medications. The sign and symptoms suggested a clinical diagnosis of intestinal obstruction. USG showed telescopy of gut loop along with its mesentry into other infraumblical region at the level of anterior superior iliac spine suggestive of ileoileal intesusception. Exploratory laprotomy was done, intussusceptions was reduced. An ileal polyp was found to be the cause of intussusceptions which was removed along with small segment of adjacent bowel and sent for histopathological examination.
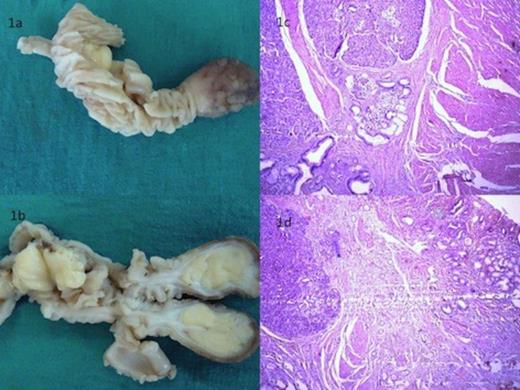
Surgical specimen of resected ileal polyp with adjacent bowel loop (1a) cut surface of which was pale yellow (1b). Histological examination revealed presence of pancreatic tissue in muscularis propria of ileum (1c) (H&E, x40) with overlying mucosa showing congestion and metaplasia (1d) (H&E, x40)
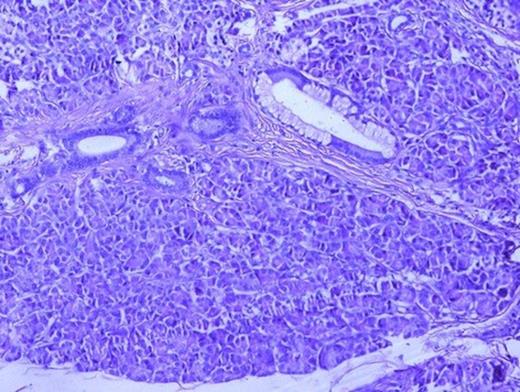
On gross examination, the polyp was brown, oval sessile mass with a broad base measuring 6×3.5×2 cm (Fig. 1a). On dissection cut surface was pale yellow (Fig. 1b). The histological examination revealed the presence of pancreatic tissue in the muscularis propria of ileum (Fig. 1c) made up of pancreatic acini and dialated ducts interspersed by smooth muscle bundles (Fig. 2). The overlying mucosa showed congestion and metaplasia (Figure 1d). Islets of Langerhans were not demonstrated.
The patient had an uneventful recovery and remains asymptomatic postoperatively.
DISCUSSION
As stated by Hunt and Bonesteel (5) the first case of heterotopic pancreas was reported by Schultz in 1729, and Klob provided its histological confirmation in 1859 (6). The reported incidence in autopsy studies is 0.5-13% (3). In adults it occurs preferentially in males between the fourth and sixth decades of life. It is found mainly in the stomach, duodenum and jejunum, in much smaller proportions in the ileum and Meckel’s diverticulum, and it is rarely found in the esophagus, liver, gallbladder, omentum, lungs, mediastinum, fallopian tubes and umbilicus (2). In adults the incidence is higher in males, while in pediatric patients the female gender prevails.
The aetiology is unknown. The proposed theory is that during rotation of foregut in a fetus and fusion of dorsal and ventral parts of pancreas, small islands of pancreas are carried away and continue to develop at its aberrant location (2).
Most patients with ectopic pancreas are asymptomatic and diagnosis is usually performed during radiological examination or endoscopy of the digestive tract or during surgical explorations motivated by other diseases (2). When symptomatic, about 30% of total mimic clinical symptoms similar to diseases that affect the organ in which the heterotopia is located (3).
Usually they present in the form of small yellowish nodules, ranging from 1mm to 5cm, typically covered by intact mucosa, and often exhibit a central hole representing exteriorization of the rudimentary pancreatic duct. However, lesions smaller than 1.5 cm do not usually show such an orifice (8). The ectopic pancreatic tissue is detected more frequently in the submucosa and muscularis propria layers of the gastrointestinal tract and may be observed in the sub-serosa or even in the serosa of the affected segment (2). The Heinrich classification system is frequently used to classify heterotopic pancreas: type 1 (containing acini, islets and ducts), type 2 (acini and ducts, no islets) and type 3 (ducts alone) (9). Our case represented type 2 heterotopic pancreas.
The diagnosis of heterotopic pancreas still remains challenging. The preoperative imaging studies (ultrasonography, endoscopic ultrasonography and computerized tomography) are not very specific (3). Hence, in the majority of cases, the diagnosis is made by histological evaluation following resection of a symptomatic or suspicious lesion (10).
When symptomatic, the lesion should be resected. The management of asymptomatic, histologically verified heterotopic pancreas or those found incidentally during other surgery is under debate. Some authors recommend resection in these asymptomatic cases to prevent later complications. Although, in the majority of the cases of heterotopic pancreas reported surgical resections were done; endoscopic mucosal removal can be an attractive, less invasive option for the resection of accessible lesions (3).
Although there have been studies describing clinicopathological analysis of patients presenting with heterotopic pancreas(2,10), ileal heterotopic pancreas has been rarely reported in children. Hereby we report one such case.
In conclusion, heterotopic pancreas is a rare congenital lesion, often diagnosed incidentally on histopathological examination and should be considered in the differential diagnosis of intestinal mass lesions.



