-
PDF
- Split View
-
Views
-
Cite
Cite
F O’Neill, M Leonard, S Morris, A bilateral crescent and anterior ring pelvic fracture sustained by inadvertently performing the ‘splits’, Journal of Surgical Case Reports, Volume 2012, Issue 9, September 2012, Page 11, https://doi.org/10.1093/jscr/2012.9.11
Close - Share Icon Share
Abstract
A case is presented of a healthy 57 year old female who slipped and fell awkwardly into what is known in athletic terms as the front splits. As a result of her fall she sustained bilateral crescent and superior and inferior rami pelvic fractures. Successful operative fixation was undertaken by a combination of open and percutaneous techniques. To our knowledge this is the first reported case of bilateral crescent fractures, and of a pelvic fracture as a result of this mechanism of injury.
INTRODUCTION
Pelvic fractures and in particular crescent fracture dislocations, which are characterised by disruption of the sacroiliac joint with extension proximally as a fracture of the posterior iliac wing, usually occur as a result of high velocity trauma (1,2). Osteopenia and the associated loss of bone trabeculae decreases the elastic resistance of the osseous elements of the pelvis, thus making the pelvis a common location for insufficiency fractures (3). As the general population ages, the number of osteopenic specific pelvic fracture patterns are likely to increase. In cases where surgical fixation is required, less invasive techniques are beneficial in this older population (3).
The unique fracture pattern described in this report occurred as a result of the patient falling in such a way as to result in simultaneous sudden flexion of one hip with extension of the contra-lateral hip, into a position known in athletic terms as the front splits. The combination of the torque force produced by the fall and the patients reduced bone mineral density resulted in a unique, unstable pelvic fracture. To our knowledge this is the first reported case of bilateral crescent fractures, and the first reported case of pelvic fracture as a result of this mechanism of injury. The authors have obtained the patient's informed written consent for print and electronic publication of this case report.
CASE REPORT
A 57 year old woman slipped while shopping resulting in a fall, where-upon her right hip flexed to 90 degrees and her left hip extended to 90 degrees, to a point where her perineum came to rest on the floor. This particular fall resulted in a twisting or torque like force being transmitted through her pelvis as she fell. She was helped up after the fall and was able to mobilise with assistance. She attributed the increased pain that she was experiencing to aggravation of her long standing back complaint. Prior to her fall she had attended the spinal clinic for her back pain and was scheduled for a bone scan with a view to progressing to facet joint blocks. On attendance at the spinal clinic following her scan it was noted that her low back pain had become more pronounced and she required walking aides in the form of crutches to mobilise. On reviewing the bone scan, multiple areas of increased uptake were noted in the bony pelvis. Further imaging, both plain film and computed tomography (CT) (Fig.1 & Fig. 2) revealed extensive pelvic fractures with displaced bilateral superior and inferior pubic rami fractures and bilateral posterior ring crescent fractures. Her past medical history was significant only for her aforementioned back pain. She had no previous fractures and prior to her fall worked as a care assistant.

Coronal computerised tomography (CT) image demonstrating bilateral posterior iliac wing fractures and sacro-iliac joint disruption
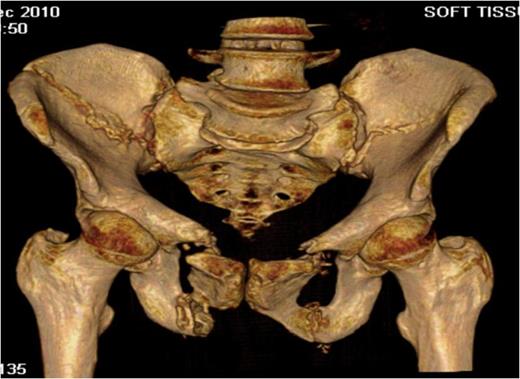
Three-dimensional CT reconstruction showing both the bilateral crescent and superior and inferior pubic rami fractures
Following admission, routine blood parameters (including bone profile) were all normal and a pelvic MRI scan out-ruled any intra-pelvic soft tissue lesions. Open reduction and internal fixation of her anterior pelvic ring was undertaken through a Stoppa approach, both rami fractures were reduced and plated anteriorly and superiorly. At this time bone and soft tissue samples from the anterior ring were sent for analysis. Following reduction and fixation of her anterior pelvis, intra-operative fluoroscopy revealed that her posterior injuries were in an acceptable position. A 3cm long vertical incision was made over both anterior inferior iliac spines and supra-acetabular screws were placed from the anterior inferior iliac spines to the posterior inferior iliac spines to fix the bilateral iliac wing fractures. Finally bilateral percutaneous sacroiliac screws were inserted to stabilise the sacro-iliac joints.

Inlet radiograph at 16 months post surgery demonstrating solid fixation and bony healing
Post-operative recovery was uneventful. Bone and soft tissue biopsies showed no abnormalities. She was kept non weight bearing for 12 weeks. Subsequent dual energy X-ray absorptiometry scanning revealed mild osteopenia for which she is being managed medically. She began full weight bearing at 3 months post surgery. Final follow-up at 16 months demonstrated that the fractures had healed, and the patient was pain free and mobilising unaided (Fig. 3 & 4).

Outlet radiographs at 16 months post surgery demonstrating solid fixation and bony healing
DISCUSSION
Pelvic crescent fractures are a relatively uncommon subtype of lateral compression injury. These injuries are rotationally unstable, there may also be some vertical displacement but this is limited by the sacrotuberous and sacrospinous ligaments, which typically remain intact (1,2). High energy trauma is usually required to cause this injury type.
Our patient sustained bilateral crescent fractures and complete bony disruption of her anterior pelvic ring through inadvertently and suddenly performing what is known in athletic terms as the front splits, where one hip is flexed and the other extended to 90 degrees in neutral adduction/abduction. Although this does not fit with the classic description of high energy trauma, the force imparted to the untrained individual’s pelvis in performing such an act would be considerable. Another contributing factor is our patients’ post-operative diagnosis of osteopenia, the associated loss of bone trabeculae decreases the pelvic elastic resistance making it a common location for insufficiency fractures in post-menopausal women (4).
Day et al (5) have classified crescent fractures according to the extent of sacroiliac joint involvement, with type I fractures entering the anterior third of the sacroiliac joint, type II fractures involving the middle third and type III fractures limited to the posterior third of the sacroiliac joint. There is no reference to bilateral crescent fractures in their classification. Operative stabilisation of these injuries is recommended and aims to achieve accurate reduction of the sacroiliac joint and stabilisation of the associated pelvic ring fracture, thus facilitating early mobilisation and minimising disability due to post-traumatic malunion and osteoarthritis or instability of the sacroiliac joint (2,3,6-9). However both reduced function and ongoing pain are commonly reported even after technically satisfactory surgery (2,7).
Pelvic insufficiency fractures are relatively common and should be suspected in older female patients with unexplained hip, groin, buttock, low back pain and/or difficulty with ambulation, particularly if there is any recent history of trauma (10). While the majority of these insufficiency fractures may be treated conservatively our patient required surgical fixation due to the unstable nature of her injury. To our knowledge this is the first reported case of bilateral crescent fractures and also of a pelvic fracture occurring as a result of this unique mechanism of injury. Operative intervention proved successful in this case.



