-
PDF
- Split View
-
Views
-
Cite
Cite
R Loh, D Foley, W Ranasinghe, K Austin, P Ranchod, R Berry, Post-traumatic pelvic extramedullary haemopoetic tissue causing lower urinary tract symptoms, Journal of Surgical Case Reports, Volume 2012, Issue 8, August 2012, Page 17, https://doi.org/10.1093/jscr/2012.8.17
Close - Share Icon Share
Abstract
Extramedullary haemopoiesis (EMH) is the abnormal development and growth of haemopoietic tissue outside the bone marrow. It is usually asymptomatic and occurs in the presence of myelodysplastic syndromes. In this report, we describe the first post-traumatic EMH presenting with lower urinary tract symptoms.
INTRODUCTION
Defined as an abnormal development and growth of haemopoietic tissue outside the bone marrow(1), extramedullary haemopoiesis(EMH) is usually a compensatory mechanism of myeloid and erythroid production outside the bone marrow and peripheral blood. This is usually due to increased breakdown or diminished production of erythrocytes, such as in myelofibrosis, thalassaemia and sickle cell anaemia (2,3). Post-traumatic EMH is extremely rare and to our knowledge, there has only been one other reported case of post-traumatic EMH (2).
CASE REPORT
We present a case of post-traumatic pelvic EMH tissue causing lower urinary tract symptoms in a 52-year-old gentleman.
He presented at the age of 19 to the emergency department after a motorcycle accident with a fractured pelvis, requiring fixation by wiring of the pubic symphysis and open reduction and internal fixation of the left acetabulum via a trochanteric osteotomy side approach(Fig. 1). He had previously experienced similar trauma, where he suffered a right hip fracture and trauma to the bowel, requiring a right total hip replacement and reparative bowel surgery, respectively.

X-ray of the pelvis showing the wiring of the pubic symphysis, internal fixation of the left acetabulum and right total hip replacement
33 years later, he presented to a urologist with 12-month history of lower urinary tract symptoms of nocturnal enuresis, urinary frequency, weak urinary stream and incomplete emptying. He had no history of urinary tract infections, but had experienced some recent weight loss. Other significant medical history included obesity, excessive alcohol consumption, paroxysmal atrial fibrillation, chronic tophaceous gout, rheumatoid arthritis, and vascular disease. His prostate was smooth on palpation, but the size was thought to be difficult to determine. This initiated a PSA test (0.29ug/L) and a subsequent ultrasound scan of the renal tract failed to demonstrate any abnormalities of the bladder or a significant post-voidal residual. However, the ultrasound scan did note an enlarged prostate of 370cc. A flexible cystoscopy was then undertaken, revealing a normal sized prostate and urethra, but noted some extrinsic compression of the bladder.
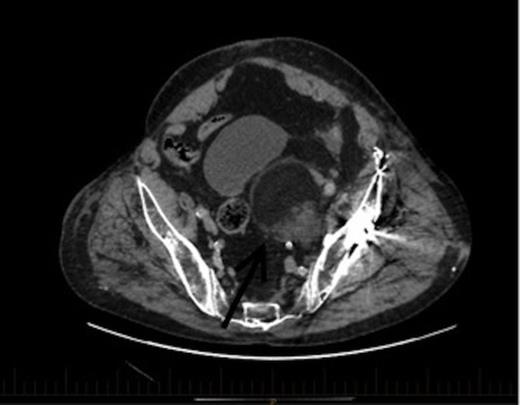
An axial section of the CT demonstrating a 6.7x6cm.3x7.3cm left pelvic lesion adjacent to the trauma site. Arrow denotes the EMH lesion
A CT scan demonstrated a 6.7x6.3cmx7.3cm well-defined left pelvic mass immediately medial and adjacent to the left acetabulum compressing the bladder and the iliac vessels. The mass was heterogeneous in density comprising of both muscle and fat with no calcifications. He underwent a repeat staging-CT, MRI, whole body thallium scan, and a CT-guided biopsy. The MRI scan confirmed a lobulated well-circumscribed mass with a heterogeneous T1 and T2 appearance. Areas of hyperintensity reported on CT corresponded to fatty components within the mass, while the rest of the mass appeared relatively hypointense to skeletal muscle, and was thought to be consistent with a liposarcoma. The Single Photon Emission Computed Tomography (SPECT) scan demonstrated low-grade activity in the mass and the staging-CT did not reveal any signs of malignancy. A confirmatory CT-guided biopsy however diagnosed the mass as EMH tissue, while a CT angiogram demonstrated no external compression of the iliac vessels.
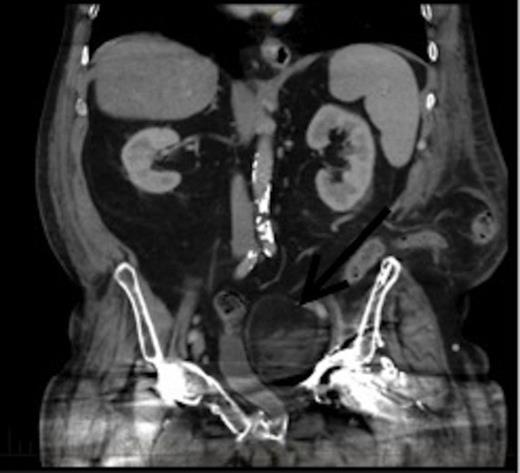
CT coronal view of the lesion demonstrating compression of the bladder. Arrow denotes the EMH lesion
This patient was subsequently discussed at a multidisciplinary meeting, where it was decided that in view of the urinary symptoms and his high operative risk, the mass should be treated with CT-guided radiofrequency ablation using a multi-lined electrode. However, the patient declined treatment and was temporarily lost to follow up after moving interstate. Two years later, he presented to the hospital with bowel obstruction secondary to an incisional lumbar hernia, and the follow up CT scan (Figures 2 and 3) revealed no increase in the size of the mass, and repeat biopsy re-confirmed the presence of EMH. His urinary symptoms remained stable.
DISCUSSION
EMH is most commonly found in the spleen, liver and sometimes in the lymph nodes. However, EMH has been reported in almost all organs in the body(1).
EMH is usually asymptomatic(4) and any symptoms are related to the location of the lesion(1). Where EMH occurs in the pelvis, patients may present with abdominal or pelvic discomfort, ascites, renal insufficiency, bladder involvement, and systemic symptoms such as fever or chills(1,4).
In this patient, EMH was diagnosed by CT, MRI, SPECT-CT scan and CT-guided biopsy. CTs commonly aid the diagnosis of EMH(3,5), and usually appears as a lobulated heterogeneous solid mass with smooth margins and similar density to that of soft tissue but slightly higher than that of fluid(3,6,7). The characteristic finding on MRI is a well-encapsulated lesion of slightly higher intensity than muscle and bone marrow on T1 and T2-weighted images, consistent with fatty tissue(3,5,8), and uniformly enhanced with gadolinium injection(3,7). Nuclear imaging using technetium-99m (99mTc) (4) and angiography (demonstrating the hypervascularity) can also be used in diagnosis of an EMH lesion(8). However, histopathological examination of tissue by CT-guided biopsy(6), ultrasound-guided biopsy(9), or diagnostic excision of the suspected mass is often essential to exclude malignancy and confirm the diagnosis(2,5,7,8). The microscopic features of EMH often reveal haemopoietic cells with polymorphous infiltrates(2,5,6), while macroscopically a soft, elastic, lobulated fatty mass is seen, usually adherent to adjacent structures, with a homogeneous erythematous cut surface(2,5,6,7).
There is limited evidence on management of this rare condition. In studies where a conservative approach was adopted, no change in the mass or adverse effect was experienced(3,6,8). However, in events of increasing pressure symptoms from the mass(3), neurological deficits(1), and anaemia due to thalassemia(10), treatment maybe necessary. Surgical resection is often reserved for symptomatic cases or when the diagnosis is uncertain(2,5,7). Due to the high efficacy and non-invasive nature, low-dose radiotherapy is also occasionally used for symptom control in EMH, as primary or adjuvant therapy to surgery(1,6). Non-surgical approaches such as hypertransfusion and iron chelation with Desferrioxamine to relieve anaemia and suppress EMH, or utilisation of hydroxyurea to stimulate fetal haemoglobin synthesis have also been described in management of EMH(10). However, their use is limited.
Extramedullary haemopoiesis as a result of trauma is extremely rare. CT and MRI scans are usually performed as part of the initial investigations. However, histolopathological examination is essential for distinguishing it from other lesions particularly malignancy. A conservative approach maybe used in asymptomatic patients, while symptomatic cases often requires surgical excision or radiotherapy. However, EMH rarely causes long-term complications.



