-
PDF
- Split View
-
Views
-
Cite
Cite
I Chawla, V Aery, K Singh, B Singla, V Singh, Duodenal tuberculosis presenting as gatric outlet obstruction, Journal of Surgical Case Reports, Volume 2012, Issue 7, July 2012, Page 13, https://doi.org/10.1093/jscr/2012.7.13
Close - Share Icon Share
Abstract
Tuberculosis of stomach and duodenum is very uncommon even in patients with pulmonary and intestinal tuberculosis. Its preoperative diagnosis still remains a challenging problem for surgeons. Herein, we report the case of isolated duodenal tuberculosis in a 42 year old male presenting with gastric outlet obstruction symptoms. Oesophago-gastro-duodenoscopy (UGIE) revealed fold thickening at D3 segment but endoscopic biopsy was inconclusive, CECT abdomen showed ill-defined soft tissue thickening involving the 3rd part of duodenum with mesenteric fat stranding. Exploratory laparotomy was done which showed growth at 3rd part of the duodenum and peritoneal seedlings, tissue biopsy was taken and gastro-jejunostomy with jejuno-jejunostomy was done. Histopathological examination was consistent with the features of gastrointestinal tuberculosis. Patient was started on anti-tubercular therapy and was cured of the disease.
INTRODUCTION
Tuberculosis is still rampant in developing countries. The most common manifestation being pulmonary disease but involvement of the gastrointestinal tract is not uncommon in these countries. Gastrointestinal tuberculosis often involves the ileocecal region. The stomach as well as the duodenum are rare sites for tuberculosis and are usually a result of secondary spread from a primary pulmonary disease. An autopsy series reported an incidence of only 0.5% (1). Duodenal tuberculosis not involving other parts of intestine is a rare entity (2).
CASE REPORT
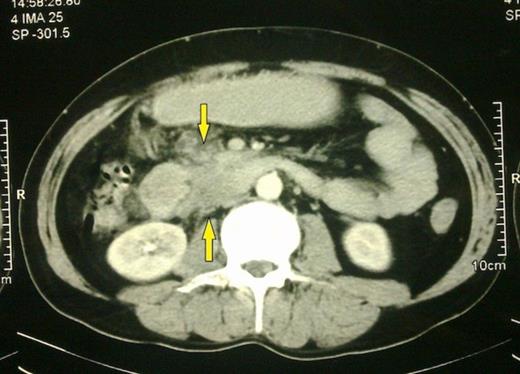
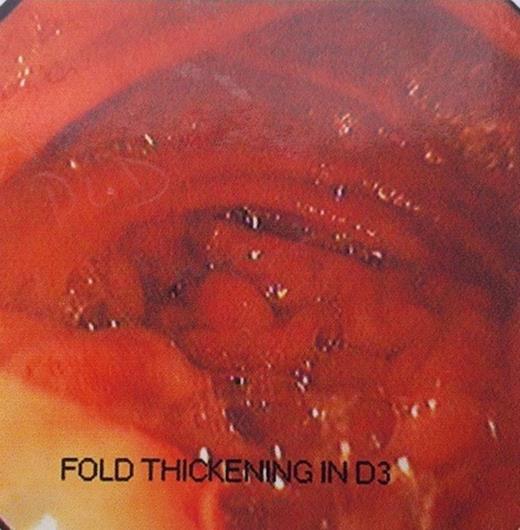
A 42 year old male presented in with pain in epigastrium since 25 days. Pain was mild in intensity, gradual in onset, continuous in nature and was aggravated on taking food and relieved on lying down. There was history of sensation of fullness after meals followed by vomiting of ingested food particles since 20 days. There was no history of fever, anorexia and weight loss, burning pain in upper abdomen, bleeding per rectum, jaundice or any urinary complaints. There was no past history of chronic cough with haemoptysis. There was no family history of tuberculosis. General physical examination was within normal limits. The USS of the abdomen was normal. However the CT showed an ill-defined soft tissue density thickening involving 3rd part of duodenum with surrounding soft tissue stranding extending to mesenteric fat with mild dilatation of proximal duodenum and stomach along with enlarged precaval nodes (Fig. 1). Upper GI endoscopy revealed a fold thickening at D3 with narrowing, scope was not negotiable beyond that part, biopsy was taken which showed lymphoplasmacytic infiltrate in lamina propria. There was no evidence of granuloma or parasite or dysplasia or malignancy (Fig. 2).
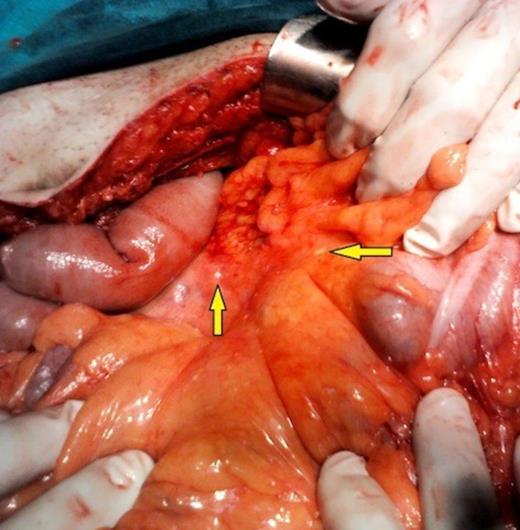
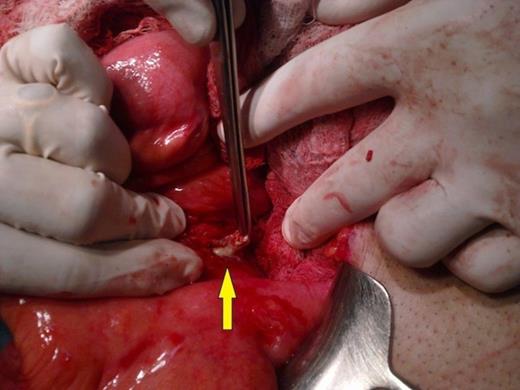
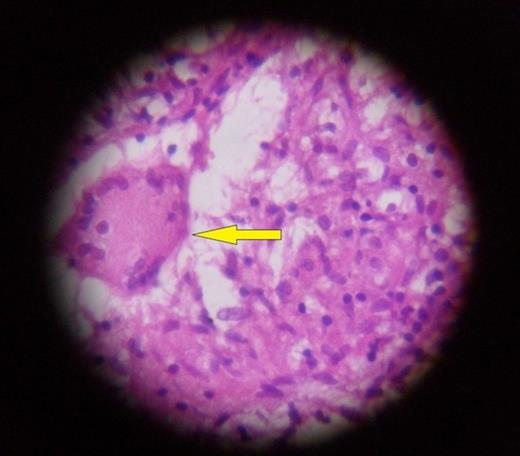
An Exploratory laparotomy was performed through midline incision. Peritoneal seedlings were seen in the mesentery (Fig. 3). A growth was seen in the 3rd part of duodenum (Fig. 4). Biopsy was taken from growth and peritoneal seedlings, following which retrocolic gastro-jejunostomy and side to side jejuno-jejunostomy were done. The remaining abdominal organs were within normal limit. Growth along with peritoneal seedlings was sent for histopathological examination. Sections from the growth showed granuloma formation along with areas of caseating necrosis and Langhans type giant cells, suggestive of tuberculosis (Fig. 5).
DISCUSSION
TB is an important medical, social and economic problem in developing countries. According to the World Health Organization (WHO), in India alone, there are 3-4 million new cases of TB every year, 2-5% of these are abdominal. It is estimated that there would be approximately 100-200,000 cases of abdominal TB in India every year. Gastroduodenal TB is uncommon even in parts of world where TB is endemic. The bactericidal property of gastric acid along with motor activity of the stomach and scarcity of lymphoid tissue in gastric wall are reasons for infrequent involvement of gastroduodenal area (3). The possible routes of infection are direct invasion through the mucosa. The most likely route in primary gastroduodenal tuberculosis is haematogenous spread, lymphatic spread and spread from the serosa by continuity from adjacent structures, especially the lymph-nodes. Duodenal tuberculosis is classified into Ulcerative, Hyperplastic, Enteroperitoneal and Infiltrative types. Gastric outlet obstruction is the most common presentation in most cases. Other symptoms are weight loss, upper GI bleeding and fever. Disease may present with fistula formation with adjacent organs, there are isolated reports of bilio-duodenal (4), aortoduodenal (5), and mesenteric artery duodenal fistula (1).