-
PDF
- Split View
-
Views
-
Cite
Cite
A Suppiah, A Dharmlingum, S Swift, AM Smith, Acute appendicitis within a recurrent inguinal hernia presenting as epididymo-orchitis, Journal of Surgical Case Reports, Volume 2012, Issue 7, July 2012, Page 12, https://doi.org/10.1093/jscr/2012.7.12
Close - Share Icon Share
Abstract
We report the first case of appendicitis within a recurrent inguinal hernia, more unique in its presentation as epididymo-orchitis. A 61-year old male presented with right testicular pain, erythematous scrotum and raised inflammatory markers. He previously had recurrent left epididymo-orchitis and right inguinal hernia repair. A diagnosis of epididymo-orchitis was made but CT was performed which diagnosed acute appendicitis within a recurrent inguinal hernia entering the scrotum. This was confirmed intra-operatively with a distal inflamed appendix segment passing beyond the medial border of the exposed mesh. Correct pre-operative CT diagnosis requires high index of suspicion even with innocuous testicular symptoms. CT reduces misdiagnosis which is associated with significant morbidity, and also aids in planning surgical approach. The only other case of acute appendicitis presenting with testicular symptoms was diagnosed only during scrotal exploration necessitating further laparotomy. The appendix entrapment beyond the mesh could suggest an alternative aetiology of mesh-related appendicitis.
INTRODUCTION
Acute appendicitis within inguinal hernia is rare but increasingly reported. We report the first case of appendicitis within a recurrent inguinal hernia. This is more unique in that it presented as epididymo-orchitis thus highlighting the need for high index of suspicion, even with innocuous testicular symptoms, following previous groin surgery. We discuss the role of pre-operative computed tomography (CT), surgical management and the possible aetiology of mesh-induced appendicitis.
CASE REPORT
A 61-year old male presented with a 12 hours of right testicular pain, scrotal erythema and raised inflammatory markers (C-Reactive Protein 324 mg/L & leukocytosis 19.9 X 109/L) on background of right inguinal hernia repair 5 years ago and more recent recurring left epididymo-orchitis. He was provisionally diagnosed with right epididymo-orchitis. CT was performed because the pain was extending to the pubic tubercle, previous hernia surgery and markedly raised inflammatory markers. This showed an acutely inflamed appendix within a small recurrent direct inguinal hernia, entering the scrotum with surrounding inflammatory soft tissue (Figure 1, 2).

Axial CT showing luminal air of appendix segment in the scotum (arrow)
A lower midline laparotomy was performed in anticipation of re-exploring the groin mesh area with a potentially difficult appendicectomy leading to possible limited caecectomy/ right hemicolectomy. CT finding was confirmed intra-operatively with the acutely inflamed appendix segment passing through a defect next to medial border of an exposed mesh segment. The appendix was delivered from within this defect and an appendicectomy was carried out without need for colonic resection. A non-absorbable suture rather than mesh was placed intraperitoneally to close the defect as the defect was small and there was concurrent appendicitis/ appendicectomy leading to potential mesh infection. Histology confirmed well demarcated distal acute appendicitis with associated fibrino-neutrophilic exudate and stromal reaction on the serosal surface. The patient made an uncomplicated recovery and was discharged 5 days later.
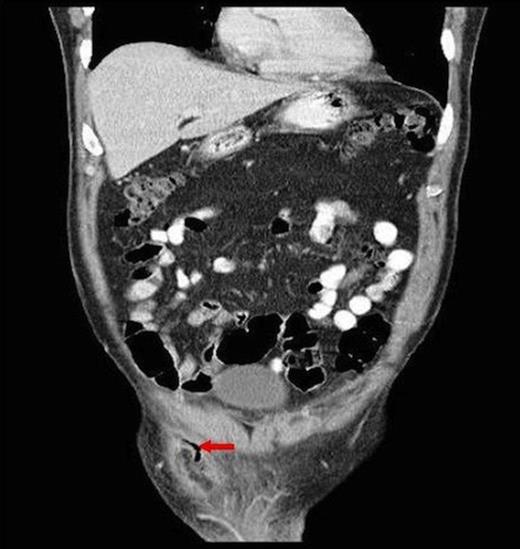
Coronal CT showing descent of appendix segment into scrotum and associated fat stranding
DISCUSSION
The incidental asymptomatic vermiform appendix is present in <1% of all abdominal wall hernia, including inguinal (Amyand) and femoral (De Garengeot) herniae. Acute appendicitis within these herniae even more rarer (0.13%) (1). Amyand hernia, named after Claudius Amyand, sergeant-surgeon to King George II, was initially described as “fistula between scrotum and thigh” in a 11-year old boy in 1736 and was also the earliest recorded appendicectomy but not recognised due to its presentation. Subsequent accreditation for the traditional appendicectomy was attributed to other surgeons including C. McBurney nearly a century later. Acute appendicitis within a recurrent inguinal hernia has never been reported, and is more unique in its presentation as epidiymo-orchitis. The presentation, aetiology, pre-operative CT diagnosis and surgical approach are discussed.
Appendicitis within a hernia most commonly presents as a strangulated hernia. The largest series of 18 patients with appendicitis within inguinal hernia reported most common presentation with painful groin lump (83%) followed by abdominal pain (11%) and small bowel obstruction (6%) but none with testicular symptoms (1). There is one reported case of Amyand hernia presenting as epididymo-orchitis, but was within a primary hernia and more importantly, the diagnosis was only made at scrotal exploration (2). Serum biochemistry is often normal because inflammation is contained within the sac, or can be raised non-specifically (as in our case) which could equally be attributed to appendicitis, strangulated hernia or epdidymo-orchitis. CT is the diagnostic modality of choice.
CT has 18 – 97% sensitivity and near 100% specificity and up to 98% accuracy in diagnosing intra-abdominal appendicitis leading to reduction in negative appendicectomies from 22% to 14% and identification of concurrent pathology in 51% in one series (3). The most common CT findings are that of enlarged appendix with surrounding fat stranding (93%) which is similar to our case (4) (Fig. 2). The only other reported pre-operative detection of appendicitis within a hernia was also diagnosed by CT (5). CT is becoming increasingly available without harmfully delaying surgery and can direct surgical approach.
Laparoscopy has been advocated as the first line approach which could confirm diagnosis, perform appendicectomy and / or hernia repair, or confirm diagnosis and plan open surgical incisions. Other authors suggest laparoscopic appendicectomy, followed by open hernia repair to avoid contamination of the hernia repair site (6). Other described treatment approaches include appendicectomy and suture / mesh hernia repair and drainage of appendiceal abscess and interval hernia repair (7). If CT is unavailable and there is diagnostic uncertainty, laparoscopy is justifiable as delayed diagnosis of appendicitis is associated with significant morbidity. Furthermore; if the appendix was normal but a hernia was present, this could be repaired. In our case, a lower midline laparatomy was performed in anticipation of performing a full groin re-exploration, difficult appendicectomy leading to a possible limited right hemicolectomy in view of the CT findings and clinical finding of a right groin mass. In hindsight, laparoscopy could have been attempted first for further evaluation. It is not possible to say if the procedure could be completed laparoscopically as there was difficulty in retrieving the appendix.
Primary acute appendicitis is thought to be caused by intra-luminal congestion and inflammation. Appendicitis within herniae is thought to be caused by extra luminal constriction by the hernia neck. The mesh provides another aetiological possibility. There is only one report of acute appendicitis related to hernia repair 18 months prior where the inflamed appendix was adherent to peritonealised mesh. The authors’ postulate appendicitis could have been caused by mesh irritation or appendix adherence to mesh with subsequent kinking leading to inflammation, or primary acute appendicitis which adhered to the old mesh site (8). The demarcation of acute appendicitis in the distal segment in this case suggests appendix entrapment as it had passed into the scrotum or adherence to the medial border of the non-peritonealised exposed mesh (Figure 2).
We present the first case of acute appendicitis within a recurrent inguinal hernia. This presented as epididymo-orchitis. We emphasise the importance of high clinical suspicion of even benign symptoms, especially if associated with previous groin surgery. Finally, we highlight the benefits of CT in avoiding missing diagnosis of appendicitis, and also planning surgical approach.



