-
PDF
- Split View
-
Views
-
Cite
Cite
RL Harries, KF Gomez, Splenic rupture following thrombolysis treatment for acute myocardial infarction, Journal of Surgical Case Reports, Volume 2012, Issue 7, July 2012, Page 11, https://doi.org/10.1093/jscr/2012.7.11
Close - Share Icon Share
Abstract
Thrombolysis is the gold standard of treatment for acute myocardial infarction (MI), however can be associated with haemorrhagic complications. To date, splenic rupture following thrombolysis has only been reported in those with an associated history of major trauma or splenomegaly. We report a case of a 47-year old female who developed splenic rupture following thrombolysis treatment with no history of trauma or splenomegaly. She received Tenecteplase therapy for an inferior MI, and six hours later she developed upper abdominal pain and hypotension. CT showed large haemoperitoneum with a large peri-splenic haematoma. She subsequently underwent a laparotomy and splenectomy. Patient remained well and was discharged home eight days postoperatively.
INTRODUCTION
Thrombolytic therapy has become the gold standard in the treatment of acute myocardial infarction (MI), in the absence of contraindications (1,2). However thrombolysis can be associated with haemorrhagic complications, with a reported incidence of between 5% and 12% (3,4). Bleeding may occur at the injection site, intra-cranially, within in the gastrointestinal tract or elsewhere, and can result in high mortality rates. This report describes a rare case of splenic rupture following the administration of Tenecteplase for an inferior myocardial infarction.
CASE REPORT
A 47-year old caucasian female developed a sudden onset of chest pain. She had no previous medical history. Risk factors for ischaemic heart disease included a 20 pack-year smoking history and her mother died following an MI aged 55 years. An electrocardiogram (ECG) performed by the paramedics showed an inferior ST elevation MI with reciprocal changes in leads V1-V3. She had no contraindications to thrombolytic therapy and therefore paramedics administered Tenecteplase. She also received an intravenous bolus injection of Heparin, Aspirin 300mg, Clopidogrel 300mg and sublingual Glyceryl Trinitrate spray. ECG changes resolved following thrombolysis.
On admission to hospital, she was haemodynamically stable. An admission Troponin level was 7.30. She was transferred to Coronary Care Unit for Heparin infusion.
Six hours later, she developed upper abdominal pain. Systolic blood pressure had dropped from 121mmHg to 89mmHg. On examination, she had a tender upper abdomen with associated guarding. Rectal examination revealed soft stool only. ECG had remained improved. Haemoglobin was found to have decreased from 13g/dl to 9g/dl, and therefore the heparin infusion was discontinued and 4 units of packed red blood cells were transfused. A surgical opinion was requested and a Computed Tomography (CT) scan of abdomen and pelvis was performed. CT showed a large haemoperitoneum with a large peri-splenic haematoma (Fig. 1).
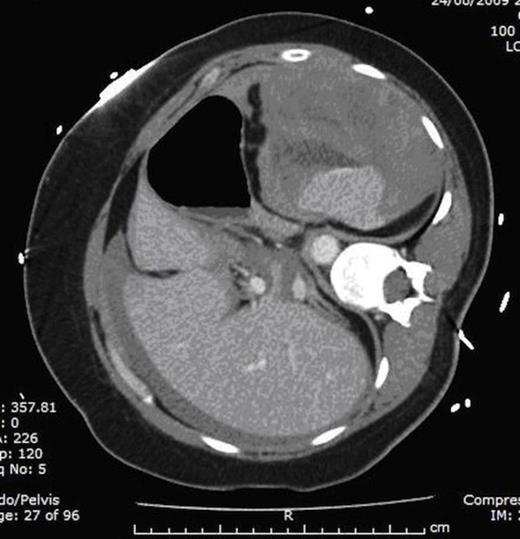
Computed Tomography (CT) of abdomen and pelvis scan demonstrating large haemoperitoneum with a large peri-splenic haematoma
Patient was consented for surgery and warned of high risk of death. She underwent a laparotomy; intraoperatively there was three litres of altered blood and clots found in the abdominal cavity and the source of bleeding found to be related from a capsular tear on the spleen. She subsequently underwent a splenectomy. She received a further 6 units of packed red blood cells, 2 units of fresh frozen plasma and 300ml of cell saver blood.
Postoperatively she was transferred to the Intensive Care Unit and was extubated the following day, and her heparin infusion was recommenced 48 hours later. She was discharged home 8 days postoperatively, and was commenced on Penicillin V as antibiotic prophylaxis. She received triple vaccinations; polyvalent pneumococcal, haemophilus influenzae b and quadravalent meningococcal/diphtheria conjugate. She underwent insertion of a coronary stent six days following discharge. Patient remained well at 3-monthly follow-up appointment.
DISCUSSION
Major bleeding is a recognized complication following thrombolysis. To date there has been few reported cases of splenic rupture following the administration of thrombolytic agents(5-8). Two of these cases were associated with a history of significant trauma prior to thrombolysis; One involved a patient who had a road traffic accident resulting in a fractured pelvic six months prior (5) and the other had experienced a fall from a ladder 6 weeks earlier (6). Splenic rupture following administration of thrombolytic agents has been reported in the presence of myeloproliferative disorders, such as polycythemia vera (7) and in those with splenomegaly secondary to infection (8). This case is unusual, as the patient had no history of trauma, myeloproliferative disorders or splenomegaly. This case illustrates the importance of close observation in all patients post thrombolysis, especially those who develop abdominal symptoms and become cardiovascularly unstable, and highlights the need for immediate surgical review in order to prevent poor outcomes.



