-
PDF
- Split View
-
Views
-
Cite
Cite
C Hamilton, SP Carmichael, AC Bernard, Laparoscopic cholecystectomy for traumatic gallbladder perforation, Journal of Surgical Case Reports, Volume 2012, Issue 6, June 2012, Page 13, https://doi.org/10.1093/jscr/2012.6.13
Close - Share Icon Share
Abstract
In trauma, laparoscopic surgery is commonly utilized as a diagnostic rather than therapeutic measure (1). Its use is often negated because of exigency or limitations in visibility due to haemorrhage. In the present case, a 35-year-old male was involved in a motor vehicle collision and arrived haemodynamically stable with abdominal pain. Abdominal CT revealed liver laceration and active contrast extravasation near the gallbladder fossa. Although angiography with embolization would normally be used, exploratory laparoscopy was performed because of concern for gallbladder injury. The gallbladder was found to be perforated and nearly completely avulsed from the fossa. Laparoscopic cholecystectomy was performed and the patient recovered uneventfully. Gallbladder perforation after trauma is typically an incidental finding during operation for haemorrhagic shock or other indication. Early diagnosis and swift surgical intervention are required, usually via laparotomy. However, when diagnosed preoperatively in the stable trauma victim, gallbladder perforation can be treated successfully with laparoscopy.
INTRODUCTION
Laparoscopy has been adopted cautiously in trauma because of unique characteristics of the injured abdomen (1). Moreover, the urgency of many trauma cases prevents the use of laparoscopy due to the time requirements of instrument preparation. In other cases, inflammation and obscure anatomy due to haemoperitoneum have proved laparoscopy to be an inconsistent tool for diagnosis and treatment of blunt trauma. Nonetheless, laparoscopy is most valuable as a tool for diagnosis and treatment of penetrating trauma or after inconclusive imaging, regardless of mechanism. In such cases, the possibility of using laparoscopy both diagnostically and therapeutically presents the same advantages over laparotomy as in non-trauma situations. Examples of therapeutic laparoscopy for trauma include diaphragm and abdominal wall repair, splenorrhaphy and splenectomy, repair of hollow viscus puncture, and cauterizing or other control of bleeding (2-6). We report herein a case of laparoscopic cholecystectomy for blunt trauma.
CASE REPORT
A 35-year-old male involved in a motor vehicle collision arrived haemodynamically stable to the Emergency Department complaining of abdominal pain. An abdominal CT revealed liver laceration and active contrast extravasation near the gallbladder fossa (Figure 1).
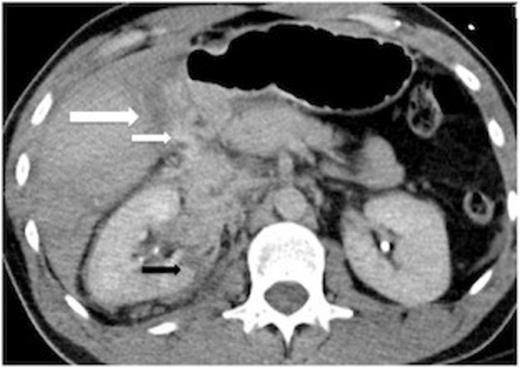
Preoperative CT scan showing a liver laceration (large white arrow) and IV contrast extravasation in proximity to the laceration (small white arrow). The normally fluid filled gallbladder is not well seen here. The right kidney is also lacerated (black arrow). There is not a large haemoperitoneum.
While hepatic contrast extravasation in a stable patient is typically treated with angioembolization, proximity to the gallbladder was concerning for gallbladder injury. Exploratory laparoscopy was performed and the gallbladder was found to be perforated and nearly completely avulsed from the liver (Figures 2 and 3).
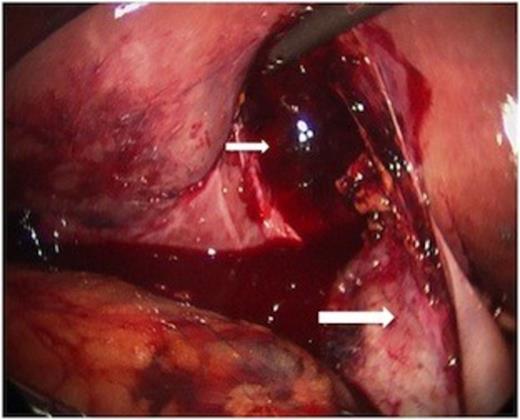
At laparoscopy, the gallbladder (large white arrow) was found partially avulsed from the gallbladder fossa (small white arrow).
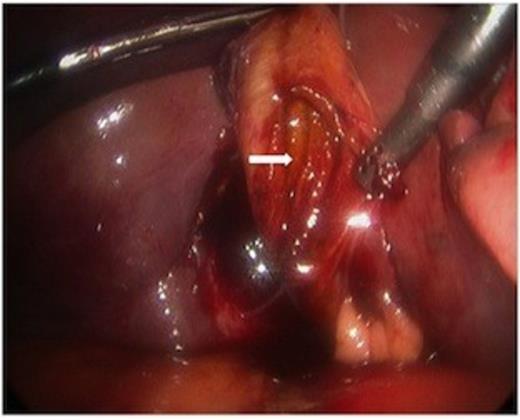
The body of the gallbladder was perforated on its inferior surface (arrow).
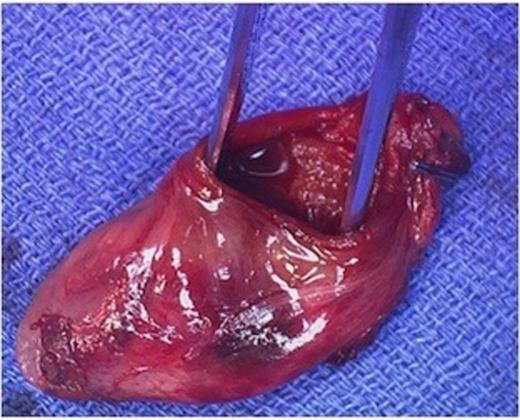
Minimal additional blunt dissection exposed the cystic artery and duct. A critical view of safety was achieved so that cholecystectomy could be performed. Only a small amount of oozing was noted from the liver laceration, following removal of the gallbladder. Haemostasis was achieved with topical agents. The pathologic specimen showed acute inflammation with perforation (Figure 4).
DISCUSSION
Laparoscopy has an established role in the diagnosis of abdominal trauma, particularly in the face of inconclusive imaging. It is most often used after penetrating trauma in stable patients, where it is considered more sensitive than CT for exclusion of visceral injury. The laceration of the liver in this case was in proximity to the gallbladder fossa and contrast extravasation here raised concern for a gallbladder injury. In this case of blunt trauma, the patient’s clinical stability and the surgeon’s ability to remove the haemoperitoneum and visualize the anatomy made it safe and feasible to manage this gallbladder injury laparoscopically. We recommend consideration of laparoscopy in trauma patients with normal vital signs in whom the initial imaging suggests pathology that can be adequately visualized within the capabilities of the equipment and skill and experience of the surgeon.



