-
PDF
- Split View
-
Views
-
Cite
Cite
AK Irving, D Gwynne-Jones, V Osipov, ML Nicholson, Juxta-articular myxoma of the palm, Journal of Surgical Case Reports, Volume 2012, Issue 6, June 2012, Page 12, https://doi.org/10.1093/jscr/2012.6.12
Close - Share Icon Share
Abstract
We present a case of juxta-articular myxoma of the hand in a 63-year-old man with an enlarging mass over the palmar radial aspect of the index metacarpophalangeal joint. Usually seen in men, this benign soft tissue tumour is normally found around large joints. To our knowledge this is the first reported case in the hand.
INTRODUCTION
Juxta-articular myxoma (JAM) is a rare, benign, soft tissue tumour with accumulation of mucinous material usually in the vicinity of large joints (1).We report a case of Juxta-articular Myxoma of the palm of the hand with imaging and histology for reference.
CASE REPORT
A 63-year-old right hand dominant male fire fighter presented to our outpatient clinic with a painless enlarging mass on the radial aspect of the base of his left index finger. It had been growing over a 12-month period. There was no history of trauma or foreign body. Physical examination showed a firm multi-loculated mass on the radial aspect of the index finger metacarpophalangeal joint extending towards the palmar surface. It was not fixed to the flexor or extensor tendons and was non-tender. The patient maintained full range of finger flexion and extension. Finger sensation was normal to soft touch and pinprick. He had an early Dupuytren’s contracture of the ring finger.
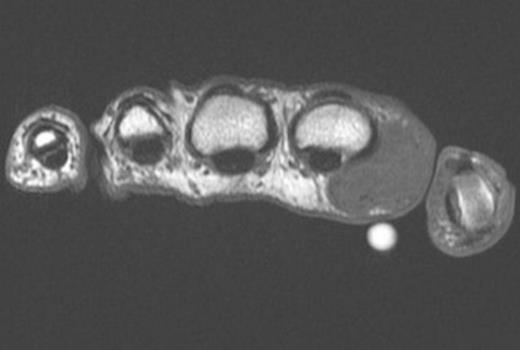
Axial T1 weighted MRI image of the mass and overlying marker (volar white circle)

Coronal Fat Suppressed Image of the mass – Depicted by the white arrow
Ultrasound scan prior to referral suggested a complex mass with solid and cystic components. MRI scan demonstrated (Figure 1 and 2) the mass to be mixed fibrous and cystic components reported by a radiologist to be either fibromatosis or a desmoid tumour. The lesion was closely positioned to the Metacarpophalangeal joint but not invading the capsule. There was no sign of osteoarthritis of the joint. A marginal excisional biopsy was performed utilizing a Bruner incision. A firm fibrous mass was found with pale coloured tissue with cystic spaces containing ganglion like jelly. The mass easily reflected off the subcutaneous dermis but deep was intimately related to the palmar fascia. The radial digital nerve and vessels were separate to the mass and preserved. The wound healed well without complication. Histopathological analysis showed an irregular mass of fibrous tissue and pale mucoid material measuring 34 x 25 x 15 mm. There were multiple cystic areas containing mucoid material. (Figure 3)
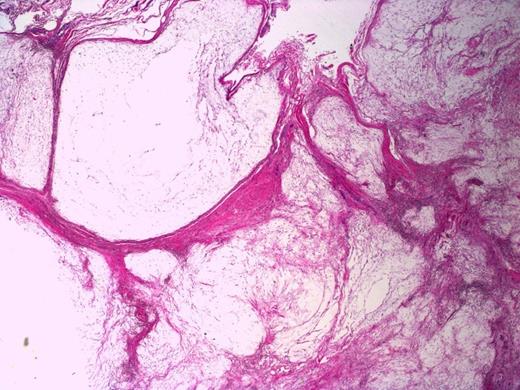
Multicystic appearance of the lesion with fibrous septa. H&E stain, 20X magnification
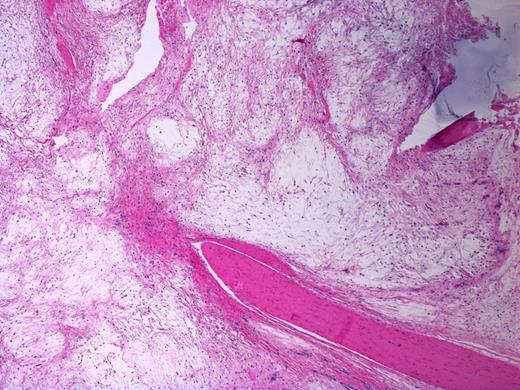
Involvement of a tendon (lower right corner) by the myxoma. Note bluish dense extracellular mucin in the right upper corner. H&E stain, 40X magnification
Sections of the lesion showed dense fibrous tissue with nodules of extracellular myxoid material containing scattered histiocytes and stellate to spindled fibroblastic cells. There was no evidence of necrosis, atypia or malignancy; this was consistent with Juxta-articular myxoma. (Figure 4 and 5). At one year follow-up there has been no sign of recurrence.
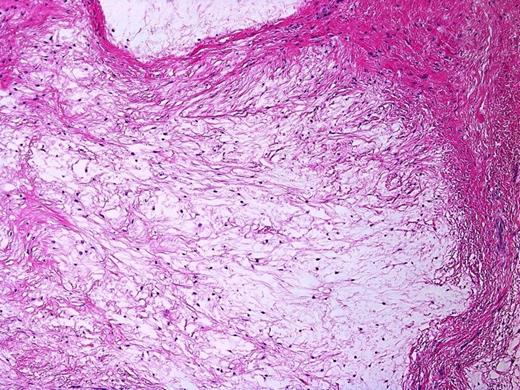
Bland spindled to stellate fibroblastic cells in a myxoid background. Note the surrounding septa composed of fibrous tissue. H&E stain, 200X magnification
DISCUSSION
More than 60 different myxoid lesions have been described (2). Histologically they are typified by copious production of extracellular mucinous material. There are 5 entities commonly accepted as myxomas: intramuscular myxoma, juxta articular myxoma, superficial angiomyxoma (or cutaneous myxoma), aggressive angiomyxoma (usually pelvic and perineal regions) and myxoma of nerve sheath (myxoid neurothekeoma). Previously intramuscular, cutaneous and juxta-articular myxomas have been regarded as one entity occurring in different locations. In a comprehensive review Allen believes, due to the differing age and sex incidence, behaviour and pathological features myxoma is not a single entity (2).
JAM is rare, at present the incidence is unknown. Ages have ranged from 5 to 83 years (3,4). It occurs more commonly in men in their 3rd to 5th decades and is usually found around the knee(3,4) but cases have been reported around the shoulder (5), elbow (6), foot (7) and ankle (4). It is not thought to be associated with any syndromes (2). There is some debate as to whether they are reactive or neoplastic (4). An association with trauma and osteoarthritis has been suggested but not proven (1). Clonal chromosomal changes have been described suggesting that at least some are neoplastic (8). The most common presentation is of swelling or mass (57 %) which may be painful (32%) (4). Initially they tend to occur in the subcutaneous adipose tissue and can be locally invasive into the joint capsule, tendons and skin (4). There is a high recurrence rate (34 %) with recurrences usually occurring within 18 months (4). The tumour macroscopically is gelatinous or slimy, soft or friable and silvery/pearly white to yellow-tan in colour (4). Histologically JAM are characterised by a richly myxoid matrix, a small number of spindle-shaped to plump fibroblast type cells and a poorly developed hypovascular pattern (2). They are histologically almost identical to intramuscular myxomasbut typically have more cystic change (2,4).
Intramuscular myxoma (IM) is a different clinical entity to JAM in several ways. They are more common in women and tend to occur in the large muscles around the thigh and shoulder. They rarely demonstrate cystic change and have a very low recurrence rate (2,4). Multiple intramuscular myxomas are associated with Mazabraud’s syndrome and McCure-Albright syndrome as well as mutations in Arg201 in the Gsα gene (8).
Previous literature suggests that myxoma is extremely rare in the hand and arm. Keoshian (1964) described a case in a 62 yr old male labourer (10). A 4 x 5.5 cm mass was found in the mid-palmar space surrounding but separate from the flexor tendons. A marginal excision was performed with no recurrence at 14 months. Tolhurst reported a recurrent case of myxoma of the palm(1). The significance of the case was of the high recurrence rate with 7 attempts at excision before amputation was undertaken due to involvement of neurovascular and tendinous structures. Fletcher described a recurrent myxoma in a 66 year old man involving the intermetacarpal space of the hand with minor recurrences over 15 years (9). These cases are not clearly JAM having no mention of close apposition to a joint and histologically not containing cystic or ganglionic components typical of JAM.
Al-Quattan in 1996 described a 1cm myxoma arising from the dorsum of the little finger in a 40 year old woman that was adherent to skin (10). He suggested a classification of upper limb myxomas based on the tissue of origin. He subsequently described an intramuscular myxoma of the adductor pollicis muscle in a 7 year old boy (10). Ozcanli in 2005 reported a case of JAM of the wrist adjacent to flexor carpi radialis insertion mimicking a ganglion cyst in a 16 year old boy. None of these cases had recurrence reported at 1 year.
The myxoma we describe most closely matches a juxta-articular myxoma near the index finger metacarpophalangeal joint. We believe this to be the first reported case of Juxta-articular Myxoma in the hand. At 12 month follow up there has been no local recurrence following marginal excision.



