-
PDF
- Split View
-
Views
-
Cite
Cite
PE Kaloostian, H Tran, Intracranial taser dart penetration: Literature review and surgical management, Journal of Surgical Case Reports, Volume 2012, Issue 6, June 2012, Page 10, https://doi.org/10.1093/jscr/2012.6.10
Close - Share Icon Share
Abstract
We report the case of a fourteen-year-old female who obtained TASER dart penetration to her right parietal region. She was neurologically intact with headache. CT scan of the head demonstrated TASER penetration intracranially without hemorrhage. Attempts were made at sterile removal of TASER at bedside under sedation. This caused the TASER to break at multiple points leaving only an intracranial component. She was urgently taken to the operating room for craniectomy for TASER removal. After reviewing the literature of an additional two patients, we suggest patients should not have attempts at removing device at bedside and should be taken to the operating room for adequate removal and washout.
INTRODUCTION
We present a case of intracranial TASER (Thomas A. Swift’s Electric Rifle, TASER International, Scottsdale, Arizona) dart penetration requiring neurosurgical management. This case demonstrated initial bedside removal to be unsuccessful. We review the literature of three cases and determine optimum management of patients with direct intracranial TASER injuries.
CASE REPORT
Our case is of a fourteen-year-old female who was running away from police and was subsequently shot in her right parietal skull with a TASER. She had initially presented to a small community hospital but was transferred subsequently to our neurosurgical unit. She complained of a moderate right parietal headache. On neurological exam, she had no deficits. She clearly had a TASER dart in the right posterior parietal skull with 4 cm of the dart visible outside of her skull (Figure 1).

CT scan of the head revealed the dart to have traversed the inner and outer tables of the skull, with a portion extending intracranially (Figure 2).
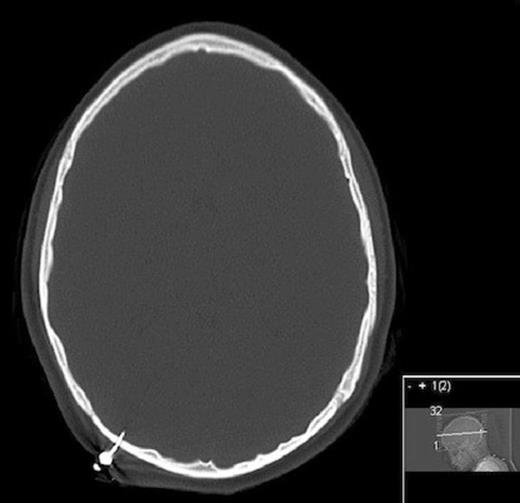
CT head bone windows showing penetration through inner and outer tables of skull intracranially
No hemorrhage was noted. The transverse sinus was not involved. Multiple attempts were made at removing the TASER dart under sterile conditions at bedside with the dart subsequently breaking, leaving only the intracranial component (Figure 3).

After attempt at removing dart at bedside in patient two, extracranial portion broke off
Patient was taken to the operating room and a craniectomy was performed for removal of the dart. It was noted that the dart traversed the entire skull leaving a small hole and was tightly adherent to the skull (figure 4). The outer layer of dura was penetrated and had a blue discoloration likely from heating, however no csf leak was noted. An appropriate sized burr hole cover was placed over the craniectomy site. The wound was washed out and the incision closed with vertical mattress sutures. The patient did well postoperatively and was discharged within two post-operative days.
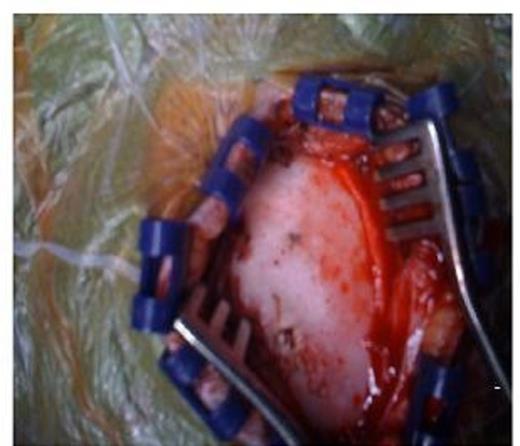
Intraoperative picture showing entry site after extracranial portion broke off
DISCUSSION
TASER devices were developed in 1974 and are energy weapons that temporarily stun a person by affecting neurotransmitter transmission. Newer TASERS have been developed since and can operate at 14 watts and deliver peak voltages of up to 50,000 volts. After the initial blast, the voltages then decrease. TASER mechanism of action is via compressed nitrogen propelling two barbed probes up to 15 feet (1). Electrical impulses are transmitted between the two probes and once striking an individual, they lose complete neural control (2).
There are only now three documented direct intracranial injuries due to TASER penetration of skull, two from our department (3) and one from University of Kansas (2). In all three cases of penetration of skull, attempts at removing the device at bedside were unsuccessful due to the complete penetration of both inner and outer tables of the skull (2). This left a foreign body lodged within the cranial vault. The goal is to remove the device entirely, in a timely fashion to diminish risk of infection, and without any associated intracranial bleeding. In the two cases at University of New Mexico (3), both patients required small surgical craniectomies for removal of skull and TASER fragment. Only one patient had direct dural penetration. These devices are so embedded in the skull that attempts at removing these at bedside have not been successful.
All patients did well post-operatively without any neurologic decline or infection. The one case at University of Kansas (2) did not penetrate the inner table of the skull. Attempts at removing the device were also unsuccessful. CT scan demonstrated a small fragment just superficial to the inner table of the skull and the decision was made to leave the fragment in. There were no complications reported from that case (2).
In all three documented cases, there was no intracranial bleeding or neurological compromise post-operatively. Based on the existing literature, if the fragment does not penetrate the inner table of the skull, we propose that the fragment may be left in place and closure of laceration on skin performed. If the dart penetrates the entire skull and possibly the parenchyma, it acts as a sharp object that may be a focus for cortical contusion and therefore should be removed via small craniectomy. It may also act as a source of infection and so neurosurgical consultation for removal of fragment would thus be recommended due to multiple risk factors.



