-
PDF
- Split View
-
Views
-
Cite
Cite
S Borude, S Jadhav, T Shaikh, SR Nath, Laparoscopic sleeve gastrectomy in partial situs inversus, Journal of Surgical Case Reports, Volume 2012, Issue 5, May 2012, Page 8, https://doi.org/10.1093/jscr/2012.5.8
Close - Share Icon Share
Abstract
Laparoscopic surgery in a patient with Partial Situs Inversus may pose interesting challenges to the surgeon. Here we report a case of a morbidly obese young female with partial situs inversus who underwent Laparoscopic Vertical Sleeve Gastrectomy (LSG). The peri-operative challenges very many and these have been enumerated. The mirror image approach is recommended in such cases for a successful surgery which was not employed in this case. Postoperative barium swallow was normal and the patient has been on regular follow up.
INTRODUCTION
Prevalence of massive obesity continues to increase and only bariatric surgery has succeeded in providing sustained weight loss (1). Laparoscopic Sleeve Gastrectomy (LSG) accounts for approximately 30% of bariatric procedures performed worldwide; and its coexistence with partial situs inversus is one in a million. Most of the global documented procedures in situs inversus involve gastric bands, gastric bypass and cholecystectomies (2). Very limited/solitary data on LSG in partial situs inversus with this being the first of its kind in India.
Situs Inversus partial is a congenital developmental anomaly wherein the abdominal organs are reversed or mirrored to the opposite side of the body through the sagittal plane. In contrast, situs inversus totalis is a similar condition in which both the thoracic and abdominal contents are reversed (2). Transmitted through an autosomal recessive inheritance, these anomalies have been in vogue since the 17th century.
CASE REPORT
A 32 yr old morbidly obese female weighing 111 Kg and BMI of 41.41 was electively admitted to the hospital. She had tried a number of diet and exercise programmes but failed to sustain reduced weight loss. She was a known case of partial situs inversus as diagnosed earlier during her pregnancy few years ago. She underwent standard pre-operative workup including physician, psychological and anaesthetic assessment satisfying our selection criteria for surgery. This Grade 3 obese patient suffered from cough, dyspnoea and chest pain. She had no history of diabetes or Ischemic heart disease though blood pressure was 130/80 mmHg. Her general examination and preoperative investigations were within normal limits. Heart sounds were normal and on the left side in the chest. Abdominal girth was increased. Preoperative barium follow through under fluoroscopic control showed situs inversus with malrotation of gut. Stomach was on the right side, normal in shape, increased size, normal mucosal pattern, no ulcer. Duodenal C Loop was opposite. Small bowel on right side and normal, no narrowing. Ileocecal junction, caecum and appendix was in left iliac fossa. Descending and sigmoid colon located on the right side close to ascending colon. CT scan of chest/abdomen and pelvis showed enlarged mediastinal lymph nodes and situs inversus. Patient was admitted one day prior to surgery and LSG was performed in January 2011. Following general anaesthesia, patient was placed in reverse Trendelenberg position. Primary operating surgeon stood on the left side of the patient as contrast to usual right side. Trocar positions were also mirror imaged. Operative feel was uncomfortable; as in a right handed person writing by a left hand. Entire upper quadrant was occupied by the liver. Enlarged spleen was in the right side. Orogastric tube negotiation was difficult because of the position of the stomach. Primary surgeon had to come to right side to reach to the right crus. Most of the time single hand technique had to be used instead of both hands. Surgical time was 90 minutes.
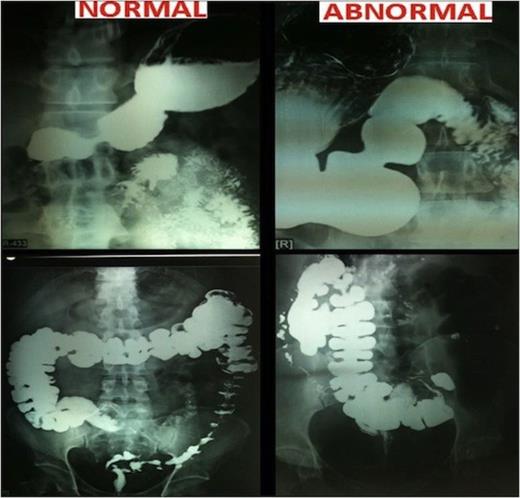
Postoperative upper GI contrast study was performed and showed no evidence of leak and a well designed vertical sleeve of the stomach. The post operative period was uneventful and patient was discharged after 4 days. She was given standard advise to remain on liquid diet for 2 weeks, followed by 2 weeks of soft diet, before reintroducing solids. Her present weight is 75Kg and BMI is 28 Kg/m2.
DISCUSSION
Situs Inversus is a rare congenital developmental anomaly with autosomal recessive inheritance wherein the position of organs in chest and abdomen are reversed along sagittal plane. The incidence of partial situs inversus in less than 1 in 22000. If associated with primary ciliary dyskinesia, sinusitis and bronchiectasis and infertility in males, it is called Kartagener Syndrome found in 25% of patients (3). Incomplete or partial situs inversus is invariably associated with cardiac abnormalities like septal defects, pulmonary arterial stenosis, tetralogy of Fallot, transposition of great vessels, and alimentary tract problems like atresia and stenosis of duodenum (4). Most of the individuals are unaware of their usual anatomy until they seek medical attention for an unrelated condition, when it is discovered incidentally. In our patient, though there was cough, dyspnoea and chest pain, routine Chest X-ray was normal as the defect involved only abdominal organs. Fortunately, the patient was aware of her condition. Our current practice involves routine chest X-ray and Sonography of abdomen.
Laparoscopic bariatric surgery in situs inversus has been reported in very few cases, wherein one patient underwent laparoscopic gastric banding (6), laparoscopic gastric bypass (5) and LSG each (3). In India, so far this case stands as the first of its kind in partial situs inversus (2,4).
Certain aspects of this type of surgery are challenging and it is recommended that an experienced laparoscopic surgeon carry out the procedure. Using a mirror image approach to all parts of the operation enabled us to successfully complete the procedure. Using this technique, our operating time was only slightly longer than normal (120 mins v/s 60 mins). LSG is thus a safe and feasible surgical procedure in situs inversus patients with very good results.



