-
PDF
- Split View
-
Views
-
Cite
Cite
S Kumar, AJ Mohan, Persistent Mullerian duct syndrome with transverse testicular ectopia, Journal of Surgical Case Reports, Volume 2012, Issue 5, May 2012, Page 9, https://doi.org/10.1093/jscr/2012.5.9
Close - Share Icon Share
Abstract
Persistent Mullerian duct syndrome (PMDS) with transverse testicular ectopia (TTE) is a rare syndrome. We report a case of PMDS associated with TTE in a 38 year old male discovered during surgery for a left inguinal hernia. Hernioplasty with excision of the persistent mullerian duct structures was done and the excised structures sent for histopathologic examination (HPE) which revealed PMDS.
INTRODUCTION
The paramesonephric duct or Mullerian duct first appears in the human embryo at the 10mm stage and begins to regress in the male due to Mullerian inhibiting substance (MIS) (1). Apart from various disorders of regression, there is also a well documented syndrome known as the PMDS, caused by the failure of regression of the Mullerian duct structures. This is a rare form of male pseudohermaphroditism, characterized by the presence of a uterus and fallopian tubes, in phenotypically and genotypically normal males. The association between PMDS and TTE is even more uncommon. Von Cenhossek in 1886 described the first case of TTE and in 1895 Jordan described the syndrome of TTE with PMDS (2).
CASE REPORT
A 38 year old married man with two children presented with a left inguinal hernia (LIH) and absence of right testis since birth. Examination of the groins showed normal phallus, LIH, empty right hemiscrotum, impalpable right testis and normal left testis. The hernia was indirect with cough impulse and reducibility. The contents felt like thickened omentum. He was diagnosed as having LIH with undescended right testis (UDT). Patient was advised LIH repair and imaging for undescended right testis. Since patient was not willing for the imaging evaluation of the right testis and insisted more on the hernia repair to be done first, he was booked for a Lichtenstein’s repair.
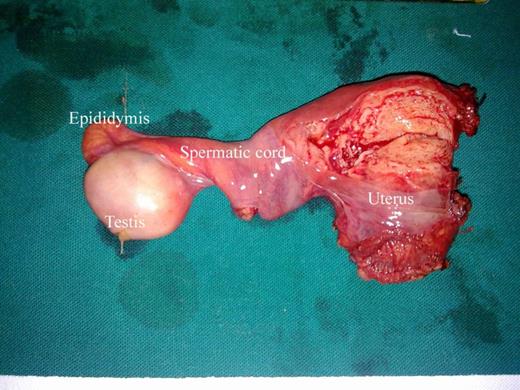
At exploration through the left inguinal incision, an irregular mass was identified within the indirect hernia sac. The sac contained two spermatic cords, separated by a rudimentary uterus, with one cornua leading to an ovary like structure (Fig.1). We thought it was uterus, fallopian tube and ovary. The entire mass was removed carefully without damaging the left spermatic cord and sent for HPE. The associated hernia was treated by Lichtenstein’s repair. We were surprised about these findings and initially had no clues, until we searched the literature and found about PMDS. The HPE report was confirmative, showing the presence of normal rudimentary uterus, testis (not ovary, as we thought) showing germ cell atrophy (Sertoli cell only), normal epididymis and spermatic cord (vas deferens).
DISCUSSION
During normal embryogenesis, differentiation of an indifferent gonad into a testis or ovary depends on the sex chromosomes. MIS and testosterone are the two principal hormones produced by the testis, the former causes the regression of Mullerian ducts, and the latter induces the development of internal male genital structures. Contrastingly, female development is an autonomous process, and does not require the presence of either gonad or hormone. Male pseudohermaphroditism results from the defective formation or action of androgens or MIS.
The male pseudohermaphrodite has male gonads and karyotype, but varying degrees of virilisation of the internal and external genital tracts. PMDS represents a small fraction of this broad spectrum of male pseudohermaphroditism, characterized by the presence of well developed or rudimentary uterus, cervix, vagina and fallopian tube in normal 46xy male.
Normally the testis is located in the scrotum at birth. Ectopic testes have been reported at various sites including superficial inguinal pouch, suprapubic, femoral, perineal region and the base of penis (3).
Migration of the testis to the opposite side where both testes pass through the same inguinal canal is known as TTE, 100 cases of which have been reported (4).
In most cases the PMDS is discovered during surgery for inguinal hernia. The pre-operative diagnosis of this condition is practically impossible. Routine pelvic ultrasound was recommended by Adamsbaum et al, in bilaterally cryptorchid patients and in patients with inguinal hernia of unusually hard consistency (5). Recently, with the advent of laparoscopic exploration of UDT, the diagnosis of TTE was possible.
In a case of PMDS with TTE, the optimal surgical approach includes tissue biopsies, hernoitomy or hernioplasty, orchidopexy and excision of Mullerian duct remnants. Some authors believe that excision of Mullerian duct structures and scrotal orchidopexy are not possible without sacrificing the vas deferens. In our patient it was possible to dissect the vas deferens from the rudimentary uterus and remove the Mullerian duct structures without risking the vas deferens. This approach is reported by many authors as it preserves the fertility of the individual (2,5,6).
There are three anatomic variants:
- A)
in the most common male type, one testis is usually foundwithin the scrotum; the uterus and ipsilateral fallopian tube are either in the inguinal canal or can be brought into it by gentle traction in the presenting testis.
- B)
in some cases, the contralateral testis and the tube are also in the hernia sac; transverse testicular ectopia can also occur.
- C)
the least common form, or female type, is characterized by bilateral cryptorchidism with testis embedded in the broad ligaments in an ovarian position with respect to the uterus, which is fixed in the pelvis (7).
In conclusion, etiopathogenesis, differential diagnosis and operative strategies in PMDS have not been completely defined. Orchidopexy is recommended, if there is no evidence of malignancy. Removal of uterus and its derivatives can be performed provided, care is taken not to damage the vas deferens, if there is some spermatogenesis. Hence, surgeons dealing with inguinal hernia should suspect PMDS in the case of adult bilateral cryptorchidism.



