-
PDF
- Split View
-
Views
-
Cite
Cite
M Abdelrahman, CM Dowling, K O’Connor, N Mayer, E Kiely, Malignant mesothelioma of the tunica vaginalis, Journal of Surgical Case Reports, Volume 2012, Issue 5, May 2012, Page 2, https://doi.org/10.1093/jscr/2012.5.2
Close - Share Icon Share
Abstract
Malignant mesothelioma of the tunica vaginalis is a rare but potentially fatal disease. Lack of characteristic clinical features and tumour markers makes the pre-operative diagnosis very difficult. A 54 year-old man with no history of exposure to asbestos presented with a short history of scrotal swelling and pain. Ultrasound revealed a suspicious nodularity involving his tunica vaginalis, suggestive of mesothelioma. Excisional biopsy revealed a malignant mesothelioma; hence the patient was treated with radical inguinal orchidectomy and hemiscrotectomy. We present a case of this rare tumour, its management and a review of the literature.
INTRODUCTION
Malignant mesothelioma (MM) of the tunica vaginalis testis is a rare but often fatal malignancy. The lack of characteristic clinical features and tumour markers makes the pre-operative diagnosis of this fatal malignancy extremely difficult. We report a case of this tumour with a pre-operative sonographic diagnosis.
CASE REPORT
A 54 year-old male farmer was referred by his GP to our radiology department for a scrotal ultrasound to investigate a two week history of right testicular pain and swelling. He was an ex-smoker and denied exposure to asbestos in his occupation. Clinical examination of the scrotum was normal except for small bilateral hydroceles. Urine examination and blood tests including HCG, AFP and LDH were within normal limits.
Ultrasound demonstrated multifocal echogenic lesions with intrinsic vascularity confined to the tunica vaginalis. These findings were felt to be highly suspicious for mesothelioma (Figure 1). Subsequently the patient had a staging CT scan of the thorax, abdomen and pelvis and this demonstrated no evidence of metastatic disease.
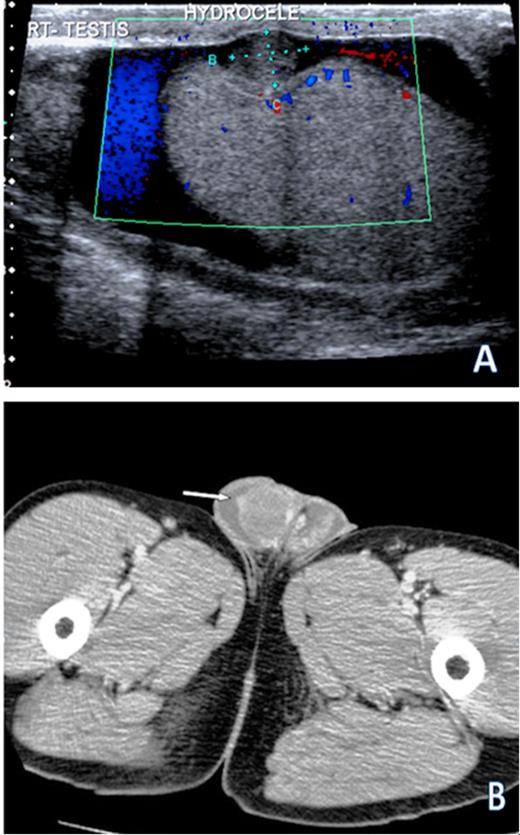
(A) Ultrasound scan demonstrating the largest of multiple small nodules studding into the right tunica vaginalis in addition to a hydrocele. Doppler interrogation suggests that this nodule has parasitized blood flow from the testis. (B) CT scan demonstrating bilateral hydroceles with enhancing nodularity of the tunica vaginalis on the right (arrow)
Following this, the patient underwent an excisional biopsy for what appeared to be a primary mesothelioma of the tunica vaginalis. At surgical exploration, there were two subcentimetre lesions on the surface of both testes. The largest on the right measured 6 mm. The lesions on the left were tiny and measured 2 to 3 mm. These lesions were excised for histology. The tiny specimens from the left side demonstrated no malignancy. On histological examination, the biopsies taken from the right testis showed a biphasic exophytic nodule composed of a mixture of epithelioid and spindled cells with mild to moderate cytological atypia (Figure 2).
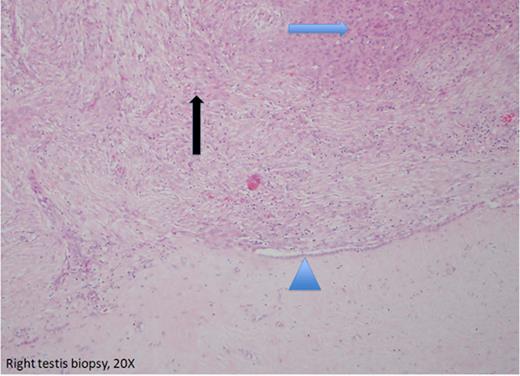
Biopsy from the surface of the right testis (20X). It shows a biphasic exophytic nodule composed of a mixture of epitheloid (blue arrow) and spindled cells (black arrow) with mild to moderate cytological atypia. A shoulder of normal mesothelial lining was included (arrow head). Occasional apoptotic and mitotic figures are present.
Occasional apoptotic and mitotic figures were also present. The morphological and immunohistochemical profile is congruent with the diagnosis of a malignant mesothelioma (Figure 3). The patient then underwent a right inguinal orchidectomy and hemiscrotectomy. There was no residual malignancy in the final specimen. A medical oncology opinion was sought and it was decided the patient should kept under surveillance with clinical and sonographic follow-up.
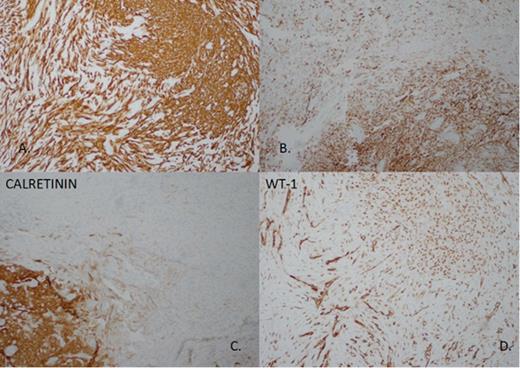
Immunohistochemistry demonstrates: A: Both epitheloid and spindled components are strongly and diffusively positive for pancytokeratin AE1/3. B: To a lesser degree both components stain positively for CAM 5.2, another cytokeratin stain. C: To epithelioid component is positive for Calretinin. D: WT-1 nuclear positivity is seen in both epitheloid and spindled components.
DISCUSSION
Mesothelioma is a neoplasm of the serosal surfaces. It involves the pleura, less frequently the peritoneum and very rarely the pericardium or the tunica vaginalis of the testis.
More than two-thirds of the cases of malignant mesothelioma (MM) are patients older than 45 years of age with the median age being 60 years (1), however it has been reported in a 10 year-old child (2). The majority of patients present with a hydrocele and some patients present with a testicular tumour. One third of these patients reported exposure to asbestos (1).
Sonographically, the most common feature of MM is a hydrocele, which can be associated with multiple extratesticular soft tissue fronds of mixed echogenicity. The hydrocele may contain multiple heterogeneous extratesticular nodular masses, ranging in size from a few millimetres to several centimetres, attached to the tunica vaginalis; or a single heterogeneous extratesticular mass arising from the scrotal wall. Less frequently, a simple hydrocele may be the only sonographic finding (1), however, appearance as a predominantly intratesticular mass has been reported (3).
Macroscopically, MM of the tunica vaginalis typically appears as multiple, firm, tan-to-white nodules or papillary excrescences on the surface of a hydrocele sac. The tunica vaginalis is usually thickened and the tumour mass may invade the spermatic cord or testis or both (3). Histologically there are 3 types of malignant mesothelioma: epithelial, mesenchymal or sarcomatous, and biphasic or mixed (4). The most frequent type found in malignant tunical mesothelioma is the epithelial type, followed by the mixed type, with the pure sarcomatous type being very rare (1,5).
Surgery is the only curative treatment for MM of the tunica vaginalis. Because most of the cases are diagnosed intra-operatively or at final histology, a second procedure is usually required to excise the remaining tissue. Radical inguinal orchidectomy and hemiscrotectomy is the recommended surgical treatment. The necessity for inguinal or iliac lymph node dissection as primary therapy remains controversial (1).
There is not enough data to support the role of chemotherapy and /or radiotherapy, however Plas et.al (1) believe that adjuvant radiotherapy should be considered for patients with locally advanced MM following tumour resection with safe margins, and for patients with metastatic disease who are otherwise fit. In their review, the common sites of metastasis were lymph nodes (13.8%), lung (9.7%) and liver (4.2%). The mean disease-specific survival for patients with or without systemic treatment was reported to be 26 and 36 months, respectively (6).
Prognostic parameters demonstrated better survival in younger age group ( < 60 years) and worse survival with the presence of metastasis. Exposure to asbestos was significantly related to shorter interval before tumour recurrence (1).
In summary, we report a case of a rare Malignant Mesothelioma of the tunica vaginalis with no history of exposure to asbestos. Our case was a pre-operative sonographic diagnosis which is unusual in this potentially aggressive tumour that lacks tumour markers and characteristic clinical features.



